More Information
Submitted: June 20, 2024 | Approved: June 28, 2024 | Published: July 01, 2024
How to cite this article: Shrivastava M. Improvement of the Cognitive Abilities in a Chronic Generalized Anxiety Disorder and Moderate Depression Case using a Novel Integrated Approach: The Cognitome Program. J Neurosci Neurol Disord. 2024; 8: 069-089.
DOI: 10.29328/journal.jnnd.1001100
Copyright License: © 2024 Shrivastava M. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Cognitive impairment; Anxiety disorder; Depression; Cognitive training; Mindfulness interventions
Improvement of the Cognitive Abilities in a Chronic Generalized Anxiety Disorder and Moderate Depression Case using a Novel Integrated Approach: The Cognitome Program
Mohita Shrivastava*
Ph.D, Founder and CEO, Cognitome Program, Cognitome LLC, Dubai, UAE
*Address for Correspondence: Mohita Shrivastava, Ph.D, Founder and CEO, Cognitome Program, Cognitome LLC, Dubai, UAE, Email: [email protected]
Cognitive impairment has been increasingly observed among patients with anxiety disorders and major depressive disorders impacting their normal daily functioning as well as quality of life. A multitude of evidence suggests that the most affected cognitive abilities are memory, attention, perception, and executive functioning in patients with anxiety and depression. Impairment in these higher-order cognitive functions can be attributed to age, education, diet, hormonal changes, stress, and prolonged use of drugs/alcohol/ medicines. To address the issues related to cognitive impairment various non-pharmacological therapeutic modalities such as Cognitive remediation approaches viz; cognitive rehabilitation, cognitive stimulation, and cognitive training; Audio-visual entrainment; mindfulness-based interventions; and neurofeedback have come into play in recent years. It is imperative to understand that the ability to test, measure, and monitor cognitive performance along with implementing cognitive remediation approaches viz; cognitive stimulation, cognitive training, etc. across the lifespan helps in early identification, accessing treatments faster, staying healthy for longer, and improving overall quality of life. This article discusses a case study of a client suffering from generalized anxiety disorder and moderate depression who after undergoing and following a novel therapeutic approach, ‘The Cognitome Program’ has shown credible improvement in cognitive abilities, along with a prominent reduction in the symptoms of anxiety, depression, and better psychological and physical well-being. Guided by the concept of neuroplasticity and cognitive plasticity, our innovative neuroscientific holistic program- ‘The Cognitome Program’ empowers unlocking hidden cognitive potential using cutting-edge methodologies and personalized strategies.
Anxiety disorder and cognitive impairment
Anxiety disorders are among the leading causes of disability and come with a variety of other medical conditions; aggravating symptoms; thereby increasing the risk for other mental disorders [1]. Generalized Anxiety Disorder (GAD) is a mental health condition that causes fear and excessive worrying along with a continuous feeling of being overwhelmed about activities of daily living. Various clinical reports have stated that there exists a comorbidity between GAD and other psychiatric disorders like Major Depressive Disorder (MDD) with observed neuropsychological impairments [2]. Moreover, even if the symptoms of anxiety do not reach the criteria for a disorder, they can cause misery and poor health posing a significant challenge to one’s mental health [3,4]. A multitude of evidence suggests that anxiety disorders, viz; GAD, and depressive disorders are usually seen as linked to impaired cognitive abilities like attention, working memory, and executive functions [5,6]. Evidence suggests that cognitive impairments such as difficulties in the ability to recall past events (episodic memory) and working memory [7]; emotional dysregulation, and emotional reactivity [8] a hallmark of anxiety disorders. In fact, DSM-V identifies cognitive dysfunction as a core symptom of depression and the prominent symptoms include (difficulty in thinking and concentrating, decision-making, and impaired memory) [9]. Moreover, difficulties in performing cognitive tasks that involve planning, problem-solving, and decision making (executive functions), learning, memory, attention, processing speed, and reaction times increase the risk of recurrence of depression [2,10]. Furthermore, anxiety can weaken the ability to engage and exploit cognitive resources [2] and make it challenging for anxious individuals to concentrate, remember information, or perform complex cognitive tasks. Further, chronic insomnia is observed among patients with anxiety disorders and insomnia-related cognitive impairment is also one of the common complaints among older adults [11]. It is evident that these higher-order functions can be affected due to age, education, diet, hormonal changes, stress, prolonged use of drugs/alcohol/ medicines, psychiatric disorders, psychological disorders, and neurological disorders [2,12]. The impact of anxiety on cognitive function is a major contributing factor to sizeable psychological, social, and economic costs [13] and fosters a debilitating focus on negative life events, making activities of daily living difficult in terms of routine learning and memory-related tasks, executive functioning leading to the problems in personal, social and work environments [14]. In spite of advances in the latest research and pharmacotherapy being used for the treatment of anxiety disorders, there still exists a significant challenge to mental health as pharmacological treatments often exhibit suboptimal efficacy as well as unwanted side effects [4,15,16]. Though there is evidence indicating the use of- cognitive behavioral therapy‐based treatments have shown small effects in improving the symptoms of depression, and the ability to manage activities of daily living (ADLs) and negligible effect in anxiety [17]. Besides, a group of researchers has indicated that supportive treatment approaches like talk therapies-guidance and counselling have not exhibited any significant effect on symptoms of depression with Mild Cognitive Impairment (MCI) and any noticeable effect on anxiety [17]. In due course, these conditions signal the need for a novel approach to improve the synergy between the brain, mind, and behavior thereby helping not only to improve mental health but also cognitive health. Therefore, in recent years, many novel therapeutic approaches involving cognitive remediation programs have been employed by clinicians/neuropsychologists/neuroscientists especially to address the issues related to cognitive functioning among patients of neurological, psychiatric, and psychological disorders. For instance, Cognitive rehabilitation, both restorative and compensatory, and cognitive training, are the most supported non-pharmacological and cognitive remediation modalities that use various therapeutic techniques to improve and restore cognitive functions in people with cognitive impairment [18,19]. Moreover, evidence also suggests that cognitive training and cognitive rehabilitation help in the improvement of cognitive functioning for cases with mild to moderate Alzheimer’s disease and vascular dementia [18]. As we are aware that our abstract and thoughtful mind and our structured brain preserve the capability for both neural plasticity and cognitive plasticity, therefore, utilizing the concept of neural and cognitive plasticity, cognitive remediation approaches viz; cognitive training have been employed to improve cognitive functioning. Evidence suggests new plastic changes in the brain can be stimulated and sustained in the aging brain by exposure to novel experiences, including education and training, optimal lifestyle factors like a healthy diet, and exercise supporting the underlying neural plasticity mechanisms [20]. A multitude of research suggests that emerging interventions viz; auditory brain wave entrainment [21,22], cognitive exercises (both manual/computer based-to improve cognitive flexibility, inhibitory control, attention, memory, goal-directed behavior) [23-25], mindfulness therapy [27], journaling and affirmation, helps to induce neuroplastic changes and cognitive restructuring and helps in the improvement of cognitive functioning including emotional intelligence and creativity. Based on these research evidence and exploiting the concept of neuroplasticity, a novel therapeutic neuroscientific program, ‘The Cognitome Program’ has been devised encompassing the holistic approach for the therapeutics and management of cognitive impairment and for the betterment of the brain, mind, and behavioral health.
The cognitome approach: ‘Care’ and ‘Cure’
The Cognitome Program specializes in improvising cognitive health. It offers comprehensive cognitive skills and executive function training, cognitive control, and rehabilitation programs. It is evident that most cognitive training programs utilize the concept of neuroplasticity (the brain’s ability to renew itself throughout life and its capacity to shape our experiences) and cognitive plasticity at functional and structural levels [20]. By employing various cognitive improvement strategies and learning techniques, the Cognitome Program prioritizes improving cognitive functions and facilitating positive changes in the brain and mind. It provides in-person as well as online assessments, management, and therapeutics. Neuroplasticity exhibits variability across individuals due to individual differences such as age, psychological factors, and neurological diseases [28]. Our tailored approach therefore focuses on enhancing cognitive abilities and optimizing brain function through targeted cognitive training and neuroscientific therapeutic interventions. Research suggests the feasibility and potential benefit of a personalized Computerized Cognitive Training (CCT) intervention to improve cognitive functioning among people [29]. The Cognitome Program following the evidence-based research includes manual/pen-paper /computer or device-assisted cognitive tasks and cognitive exercises [23,24], mindfulness-based interventions [26,30] for the improvement of impaired cognitive abilities as well as improving emotional and creative intelligence. It may or may not be the same for two individuals due to individual differences, demographics, types of issues, causes and related disorders and their own willingness Cognitome Program is comprised of Plan CARE (Consultation, assessments, results, and evaluation) and Plan CURE (Customized, Unique, Relevant and Enriching). Plan CARE includes multiple tests and assessments based on the type of disorder and domain to be assessed. It encompasses consultation and obtaining initial information; detailed assessments; analysis of results and evaluation of reports. Plan CURE is a customized therapeutic plan aiming to address the issues specific to the client, devising a plan of action after careful assessments and evaluation of the results, and implementing the plan thereof with modifications based on real-time feedback thereby promoting cognitive restructuring and neuroplastic changes.
Background
FP-33CV (Identity kept confidential as a part of the moral and ethical code of conduct of the Cognitome Program) is a 50-year-old, right-handed southeast Asian female who migrated to Dubai, UAE in 2010. She is a single mother of 4 grown-up boys who carries the responsibility for the upbringing/education of her children. She has been working as a senior teacher in a Kindergarten School for the past 10 years. She is well-educated in terms of the degrees and diplomas required for her job. She also keeps on updating her set of knowledge and skills by participating in continuous workshops as needed for her job skills. She is a God-fearing, religiously inclined, hardworking, and disciplined female. She has neither used any illicit drugs nor is inclined to alcohol abuse. She takes medications for her lower back pain/neck shoulder pain along with Physiotherapy sessions as prescribed and advised by her medical physician. She has also taken multivitamin/calcium/magnesium/iron supplements for the past 1 year and iron supplements for the past 5-6 months.
Presenting problems
Client FP-33 CV has complained of sleeplessness (insomnia), often worrying, getting anxious, sometimes feeling sadness/crying, neck and shoulder pain, low back pain, headaches, menopausal syndrome, iron deficiency anemia, and moderate to high cognitive deficit, especially in terms of processing speed, problem-solving, attention, cognitive flexibility (updating), inhibitory control (inhibition), memory, perception and perceptual abilities with bouts of confusion at times (Brain fog).
Client’s view of the problem/symptoms
The client has related her problems to different issues:
a) Generalized stress and high work demand at the workplace
b) Menopausal hormonal imbalances
c) Her own history of responsibilities/struggle
Observations during assessments/interview
The client was interviewed initially for her case history, demographic details, and current problems. During the interview, the client was awake and alert. During her tests and assessments, the client was awake, alert, focused, and followed the instructions carefully. She mentioned that she had slept for more than 5 hrs the previous night.
A comprehensive assessment protocol under the Category- CARE (Consultation, Assessment, Results and Evaluation) plan of the Cognitome program was employed. The CARE Plan was administered in stages.
Step 1: Client FP-33CV was interviewed initially to understand the status of the persisting problems. The client was then asked to give detailed information about the background, history, and demographics in the client’s initial evaluation sheet (C-IES). The client was given 48 hours to fill out the C-IES.
Ethics and confidentiality: The Client consent and confidentiality forms were considered an integral part of the ethics code of the Cognitome Program.
Declaration of ethical considerations and consent forms
All procedures followed were in accordance with the ethical standards of the National Academy of Neuropsychology, in line with the revised APA Ethical Principles and Code of Conduct (2002), to provide informed consent to patients seeking services at Cognitome LLC and views its conveyance as a basic professional and ethical responsibility. The participant and their legally authorized representative provided written informed consent before entering the study in compliance with the applicable local regulations as well as by considering the Helsinki Declaration of 1975, as revised in 2000.
Client’s declaration: As per the cognitome program, cognitome LLC’s protocol
I understand that the findings and clinical approach taken in this case may be included/shared as a part of the therapeutic protocol with the neuroscientific and medical fraternity in the larger interest of the clients/patients with similar issues. This could be in the form of a case study/exhibit/presentation/discussion/article and will be done while maintaining the personal details of the client confidential. I believe that this will benefit the needful society, the neuroscientific community, and medical fraternity.
Confidentiality and privacy of personal information as per cognitome program, cognitome LLC’s protocol
All communications with Cognitome LLC and all records relating to the provisions of cognitive training and assessment services are confidential and may not be disclosed without a client’s (or guardian’s) written consent. The privacy of your personal information is an essential and important undertaking and must be contained in the appropriate uses and protection as per the APA 2002 protocol.
Step 2: Careful evaluation and analysis of C-IES were done and the required tests/assessments/batteries (pen paper based/computer based) were employed for the comprehensive evaluation of GAD and related depression, cognitive profiling for cognitive skills and cognitive functions, lateralization of functions, spiritual and religious inclination, using reliable and validated psychological/ neuropsychological/psychological tests/batteries used globally. Assessments were done in three stages on the same day.
Step 3: Detailed analysis of results was done within 3 days of the assessment and a comprehensive report was discussed with the client along with the Plan of Action to be followed (Table 1).
Table 1: Mentioning the scores of the tests and assessments done for Anxiety/Depression/Cognitive skills/abilities before the Cognitome Program and improvement in the scores after the Cognitome Program indicating the effectiveness of the modalities employed in the Cognitome program.
| Table 1: Tests/assessments done before and end of the cognitome program. | |||
| Tests/ Assessments |
Test Scores (Before Cognitome Program) |
Test Scores (After Cognitome Program (3.5 Months) |
Inference |
| Anxiety and Depression Assessment | |||
| HAM-A | 27 | 11 | Reduction in the symptoms of anxiety |
| HAM-D | 20 | 12 | Reduction in the symptoms of depression |
| Becks Anxiety Inventory | 29 | 12 | Reduction in the symptoms of anxiety |
| Becks Depression Inventory | 23 | 13 | Reduction in the symptoms of depression |
| GAD-7 | 18 | 9 | Reduction in the symptoms of anxiety |
| DASS-21 | Anxiety: 18; Depression:11 Stress: 14; Total Score: 43 |
Anxiety:10;Depression:7 Stress: 10; Total Score:27 |
Reduction in the symptoms of anxiety, depression, and stress |
| 16 Items QoL SCALE | 53 | 74 | Improvement in QoL |
| Spiritual And Religious Inclination | |||
| Spirituality Index of Wellbeing | Self-efficacy:27 Life Skills:26 |
Self-efficacy:28 Life Skills:27 |
Spiritual inclination (Very High) |
| Centrality of Religiosity Scale | 78 | 80 | Religious inclination (Very High) |
| Cognitive Profile Tests (ManuaL and Computer-based) | |||
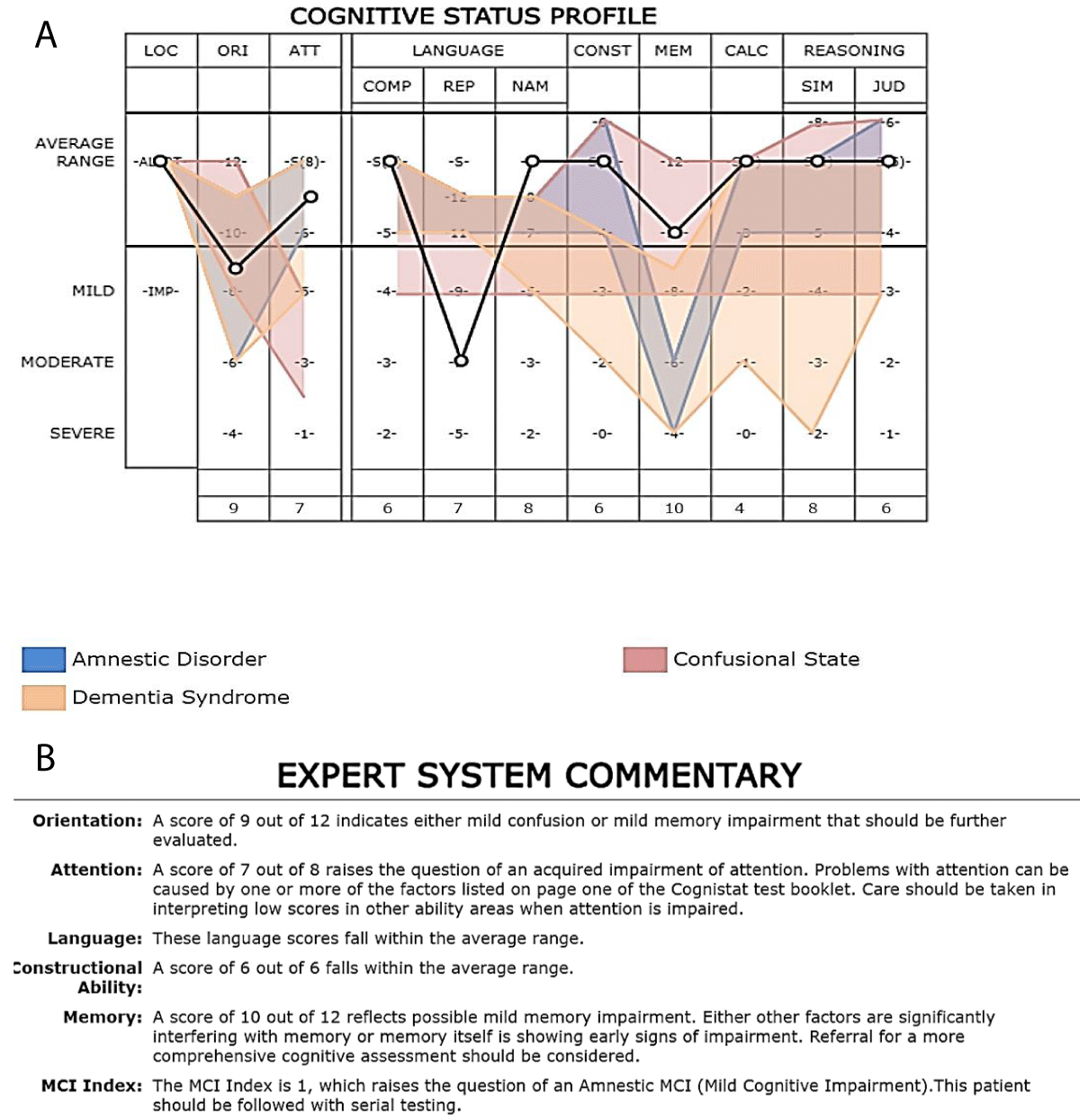
| COGNISTAT CAS II | Poor orientation, attention, and memory with an MCI index of 1 | Improvement in these domains | Improved cognitive domains |
| COGNIFIT CAB-PRO | 233.2 | 336.8 | Improvement in overall cognitive abilities |
| Cognitive Assessment Questionnaire | 62 Forgetfulness 36 Distractibility 53 False Triggering |
33 Forgetfulness 28 Distractibility 33 False Triggering© |
Reduced symptoms © |
| MMSE/ SLUMS/MoCA | 27/28/27 | 29/30/28 | Normal: No significant difference |
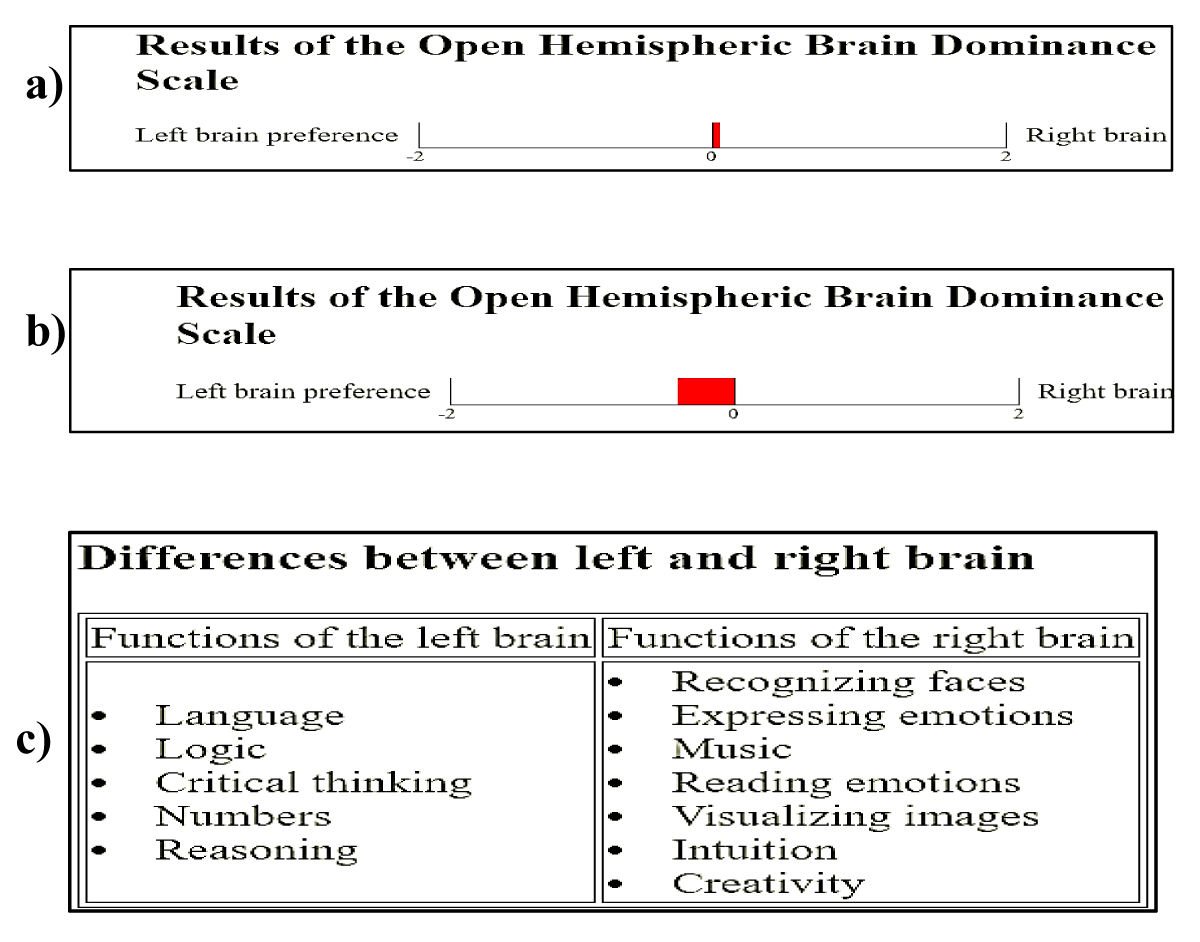
| OPEN Hemispheric Dominance Scale | 0.4 Right Hemispheric Brain Dominance | -0.8 Left Hemispheric Brain Dominance | Better Logical and Reasoning abilities |
Anxiety and depression
Assessments and tests done for anxiety: Anxiety was measured by the Hamilton Scale; GAD-7; Beck’s Anxiety Inventory, a self-report measure of anxiety scale; and Depression Anxiety Stress Scale-21 (DASS-21) by exploring the interruption of the emotional continuum and subjective sensations of tension, restlessness, or nervousness.
Hamilton Anxiety Scale (HAM-A): HAM-A scale is made up of 14 items that assess physical, mental, and behavioral symptoms characteristic of anxiety [31], evaluating both their frequency and intensity, of which 7 measure psychological anxiety (1–6 and 14) and the other 7 somatic anxiety (7–13), evaluated from 0 to 4 following the scale 0 = Absent, 1 = slight, 2 = moderate, 3 = severe and 4 = very serious. The total score ranges between 0 and 56 points. A higher score indicates a higher intensity of anxiety.
Beck’s Anxiety Inventory (BAI): BAI scale is made up of 21 items, was moderately correlated with the revised Hamilton Anxiety Rating Scale (.51), and mildly correlated with the Hamilton Depression Rating Scale (.25) [32]. The total score is calculated by finding the sum of the 21 items. Score of 0-21 = low anxiety Score of 22-35 = moderate anxiety Score of 36 and above = potentially concerning levels of anxiety. GAD-7 includes self-report subjective questions and is used to assess the common symptoms of generalized anxiety disorder for the past 2 weeks-4 weeks and the scores of anxiety levels are interpreted as follows: GAD-7 score of 0-4 (none), 5-9 (mild), 10-14 (moderate), and 15-21 (severe) [33].
Depression: Tests and assessments
Depression was measured by the Hamilton Depression Scale, Beck’s Depression Inventory, and Depression Anxiety Stress Scale-21 (DASS-21) by exploring the interruption of the emotional continuum and subjective evaluations of sadness, discouragement, failure, guilt, punishment, lack of motivation, mood, suicidal ideation, insomnia, agitation, dissatisfaction, and somatic symptoms.
Hamilton Depression Scale (HAM-D): The HDRS (also known as the Ham-D) is the most widely used clinician-administered depression assessment scale [34]. The original version contains 17 items (HDRS17) for evaluating symptoms of depression in adults, for measuring depression severity, and as a tool for monitoring changes in depressive symptoms over the course of treatment. For most questions, scores range from 0 to 4, with 4 representing more acute signs of depression. Several questions have ranges that extend only as high as 2 or 3. A total score is calculated by summing the individual scores from each question. Scores below 7 generally represent the absence or remission of depression; Scores between 7-17 represent mild depression; Scores between 18-24 represent moderate depressions; Scores 25 and above represent severe depression.
Beck’s Depression Inventory (BDI): The Beck Depression Inventory (BDI) is a 21-item, self-report rating inventory that measures characteristic attitudes and symptoms of depression [35]. The highest possible total for the whole test would be sixty-three and the lowest possible score for each question is zero, the lowest possible score for the test would be zero. A score between 1-10 ups and downs is considered normal; 11-16 Mild mood disturbance;17-20 Borderline clinical depression; 21-30 Moderate depression; 31-40 Severe depression; over 40-Extreme depression.
Depression Anxiety Stress Scale-21 (DASS-21): DASS-21 is a quantitative measure of distress along the 3 axes of depression, anxiety, and stress. There are seven items allocated to each subscale. Depression subscale: assesses symptoms such as dysphoria, hopelessness, devaluation of life, self-deprecation, lack of interest/involvement, anhedonia, and inertia. Anxiety subscale: evaluates symptoms such as autonomic arousal, skeletal muscle effects, situational anxiety, and subjective experience of anxious affect. The stress subscale measures symptoms related to difficulty relaxing, nervous arousal, being easily upset/agitated, irritable/over-reactive, and impatience. Scores are presented as a total score (between 0 and 63) and a score for the three subscales (between 0 and 21) [36,37]. The cut-off scores have been developed for defining mild/moderate/severe/ extremely severe scores for each DASS scale. DASS can lead to a useful assessment of disturbance, for example, individuals who may fall short of a clinical cut-off for a specific diagnosis can be correctly recognized as experiencing considerable symptoms and as being at high risk of further problems [37].
Quality of Life Scale
Quality of Life Scale (QOLS) was used to assess and evaluate the current state of the client’s overall well-being and quality of life. QoL is 16 items self-administered questionnaire rather than the 15 found in the original Flanagan version. Item #16, “Independence, doing for yourself” was added after a qualitative study indicated that the instrument had content validity in chronic illness groups but that it needed an item that reflected the importance to these people of remaining independent and able to care for themselves. The instrument is scored by summing the items to make a total score. The number of responses to each question ranges between 1 to 7, and each item ranges from a minimum of 16 to 112 points, with higher being a better quality of life [38,39].
Spirituality and religiosity scale
Clients’ spiritual and religious inclinations were evaluated using the following scales:
Spirituality Index of Well-Being (SIWB): Evaluates a sense of meaning or purpose from a transcendent source. It is a 12-item instrument that measures one’s perceptions of their spiritual quality of life. The scale is divided into two subscales: (1) self-efficacy subscale (items 1-6) and (2) life-scheme subscale (items 7-12). Each item is answered on a 5-point scale ranging from 1 (Strongly Agree) to 5 (Strongly Disagree) [40].
Centrality of Religiosity Scale (CRS): The Centrality of Religiosity Scale (CRS) is a measure of the centrality, importance, or salience of religious meanings in personality. It measures the general intensities of five theoretically defined core dimensions of religiosity. The dimensions of public practice, private practice, religious experience, ideology, and intellectual dimensions can together be considered representative of the total religious life [41]. The response modalities for items 1 and 2 range from 1 to 5, i.e., never- too often. Response modalities for item 3 range from 1 to 5, i.e., not at all too much. The response modality for item 4 varies from 1 to 6, i.e., never to -more than once a week. The response modalities for item 5 range from 1 to 8, i.e., never to several times a day. The scale score results from the average value of the answers, giving rise to three distinct groups: very religious individuals (scoring between 4 and 5 values), religious individuals (scoring between 2.1 and 3.9 values), and non-religious individuals (scoring between 1 and 2 values) [42].
Cognitive profile: Tests and assessments for cognitive impairment and cognitive skills/functions
Cognitive impairment: Cognitive impairment if any was assessed using the following validated tests used globally (Mini-Mental State Examination-MMSE; Montreal Cognitive Assessment-MoCA; Saint Louis University Mental Status Examination- SLUMS and Cognitive Assessment Questionnaire.
Mini-mental State Examination (MMSE): MMSE was used to measure global cognitive function [43]. It is designed to detect severe cognitive deficits and consists of a total of 30 items that comprise 5 cognitive areas: orientation, registration, language, memory, and calculation. The total score for this test is 30 points, with higher scores indicating better overall cognition on the part of the subject. Reference scores are dementia: 9 to 12; deterioration: from 12 to 24; pathological suspicion: 24 or more; normal: 27 or more.
Montreal Cognitive Assessment (MoCA): MoCA is a short test composed of 12 items that assess cognitive function through 7 cognitive domains: visuospatial and executive function (task B of tracing (1 point), copy of the cube (1 point) and clock drawing (3 points)), denomination (3 points), attention (forward/towards behind), digit interval (2 points), vigilance/tapping (1 point) and subtraction from series (3 points), language (repetition of sentences (2 points) and verbal fluency (1 point)), abstraction (the element 2-element verbal abstraction, total of 2 points), delayed recall/short-term memory (5 points) and orientation (6 points). The maximum MoCA total score is 30, and values ≥ 26 indicate normal cognitive functioning [44].
Saint Louis university mental status examination slums: The SLUM test may help people identify signs of dementia and mild cognitive impairment. SLUMS tests evaluate memory, attention span, visual-spatial function, orientation, level of awareness, and executive functioning. The test contains 11 questions and a total of 30 points. For individuals who have completed a high school education, the SLUMS score structure is as follows: 27–30: Indicates regular cognitive function; 21–26: Indicates mild cognitive impairment; 1–20: Indicates dementia [45].
Cognitive assessment questionnaire: The cognitive assessment questionnaire, originally called the Cognitive Failures Questionnaire (CFQ) was developed by Broadbent, et al. [46] to assess the frequency with which people experienced cognitive failures, such as absent-mindedness, in everyday life - slips and errors of perception, memory, and motor functioning. The most straightforward way to score the scale is simply to add up the ratings of the 25 individual items, yielding a score from 0-100 [46]. A study by Rast, et al. [47] indicates that the CFQ items load on three different factors. Adding scores across the relevant items will yield subscale scores representing dimensions of forgetfulness, distractibility and false triggering.
Brain dominance test: Brain hemispheric dominance was assessed using the Open Hemispheric Brain Dominance Test to understand the inclination or choices in terms of assigned hemispheric functions of the brain which in turn helps to understand the creative nature or logical nature of the client.
Open hemispheric brain dominance test: The Open Hemispheric Brain Dominance Scale was developed to meet the need for a free and open-source measure of the so-called “right brain”/”left brain” personality distinction [48]. The OHBDS was developed by selecting items based on correlations with five diverse other scales purported to measure the construct: the Alert Scale of Cognitive Style, the Wagner Preference Inventory, Philip Carter’s test, Madeline Turgeon’s questionnaire, and the Polarity Questionnaire. The inventory consists of 24 items that must be rated on how much you agree with them on a five-point scale where 1=Disagree, 3=Neutral, and 5=Agree. It should take most people 3 to 5 minutes to complete.
Cognitive skills/Functions tests: Cognifit Cognitive Assessment Battery (CAB): Cognitive skills tests were done using Cognifit’s Cognitive Assessment Battery-CAB-Pro a comprehensive online neuropsychological battery of 17 non-invasive tests that provide a broad, objective, and precise assessment of 22 well-documented cognitive skills.
Cognifit Cognitive Assessment Battery (CAB): Cognitive assessment is a common process in educational, clinical, or research settings, and in post SARS-CoV-2 health crisis, the pencil-and-paper format is becoming increasingly outdated and transition to new technologies, using Computerized Cognitive Assessments (CCA) is increasingly seen [25]. CAB-Pro is one such brief but comprehensive online neuropsychological battery of 17 non-invasive tests that provide a broad, objective, and precise assessment of 22 well-documented cognitive skills. The Cognitive Assessment Battery (CAB) quantitative results report a global score for gauging overall cognitive function, individual scores on 22 cognitive skills, and a well-being score. The CAB assessment also has a validity index of its measurements, and it accurately captures human cognitive development across the lifespan. It has a variable length of 30 to 40 minutes. It can be applied to computers, tablets, and smartphones. CogniFit’s highly automated platform facilitates both individual and large-scale data collection and allows for the simultaneous testing of large numbers of people. The Cognitive Assessment Battery (CAB) consists of a selection of 44 questions, 17 neuropsychological tasks, and 22 cognitive abilities. CAB is a self-administered online general cognitive evaluation psychometric tool that evaluates a variety of different cognitive abilities, placing a heavy focus on executive functions obtaining a gender- and age-adjusted general score, which ranges from 0 to 800 points, as well as five different sub-scores based on the cognitive domains of perception, attention, memory, coordination, and reasoning. A description of the 17 tests is presented as Supplementary Material. [29,49,50] (CogniFit Inc., San Francisco, CA, USA; https://www.cognifit.com/cab).
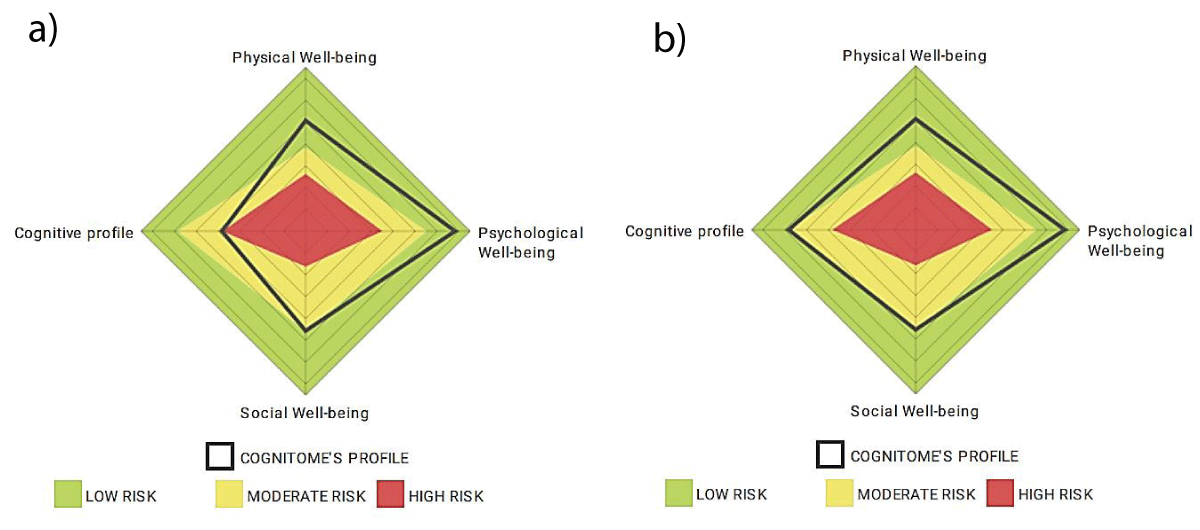
a) CAB-PRO Well-Being Questionnaire include General Questions • Physical Well-Being Questions • Psychological Well-Being Questions • Social Well-Being Questions
b) CAB-PRO Neuropsychological Tasks includes: Tapping Test • Psychomotor Vigilance Test • Number-Size Congruency Test • Digit Span Test • Time Estimation Test • Eye-Hand Coordination Test (Fixed Trajectory and Predictable Direction) • Maze Test • Visual Memory Test • Stroop Test • Eye-Hand Coordination Test (Multidirectional and Unpredictable Direction) • Visual Working Memory Span Test • Naming Test • Multimodal Lexical Memory Test • Lexical Memory Test • Speed Estimation Test • Distance Estimation Test • Divided Attention Test
Cognitome program - plan cure: Therapeutic modalities employed
Cure plan: The CURE plan (Customized, Unique, Relevant, Enriching) was administered in 3 stages of 33 days each (excluding the time of the initial interview and detailed assessments ~7 days). The execution of the plan was monitored weekly and updated periodically as per the progress of the client. The final assessments were done after the end of the third stage of the Plan. Research suggests the feasibility and potential benefit of a personalized Computerized Cognitive Training (CCT) intervention to improve cognitive function among people [29].
CURE Plan for FP-33CV: The Plan included both manual – pen paper and computer/device-assisted tasks and exercises for the improvement of impaired cognitive abilities. CURE plan was comprised of cognitive exercises- manual tasks and computer/tablets assisted exercises for cognitive skills training; brain wave entrainment- using equisync binaural waves; Cerebration techniques -Cognoscere and Emovere meant to enhance creative and critical thinking as well as emotional intelligence; Mindfulness-based interventions such as individualized meditation protocols based on spectral-light, acoustics, sensory elements/perceptual processes and real-time neurofeedback- using Muse 2 headband and Muse application. Besides, holistic approaches- bibliography sessions, educational presentations, awareness talks, mind pruning exercises, visiting natural habitats, and a mindful diet were also advised and implemented. The CURE plan devised was flexible, and tailored to the client’s issues after the careful analysis and evaluation of the assessment results (Table 2).
Table 2: Mentioning in detail the various modalities employed in the CURE plan of the Cognitome Program along their respective time frames, and use in improving overall mind, brain, and behavioral health.
| Table 2: Therapeutic modalities: plan cure of the cognitome program. | ||||
| Plan Cure: The Cognitome Program | ||||
| Modalities | *Stage | Protocol | Duration | Inference |
| Cognitive skills training | I, II, and III |
|
3 months: CB thrice a week for 12 weeks PP twice a week for 12 weeks |
Memory, focus, processing speed, reaction time, inhibitory control, and mental flexibility |
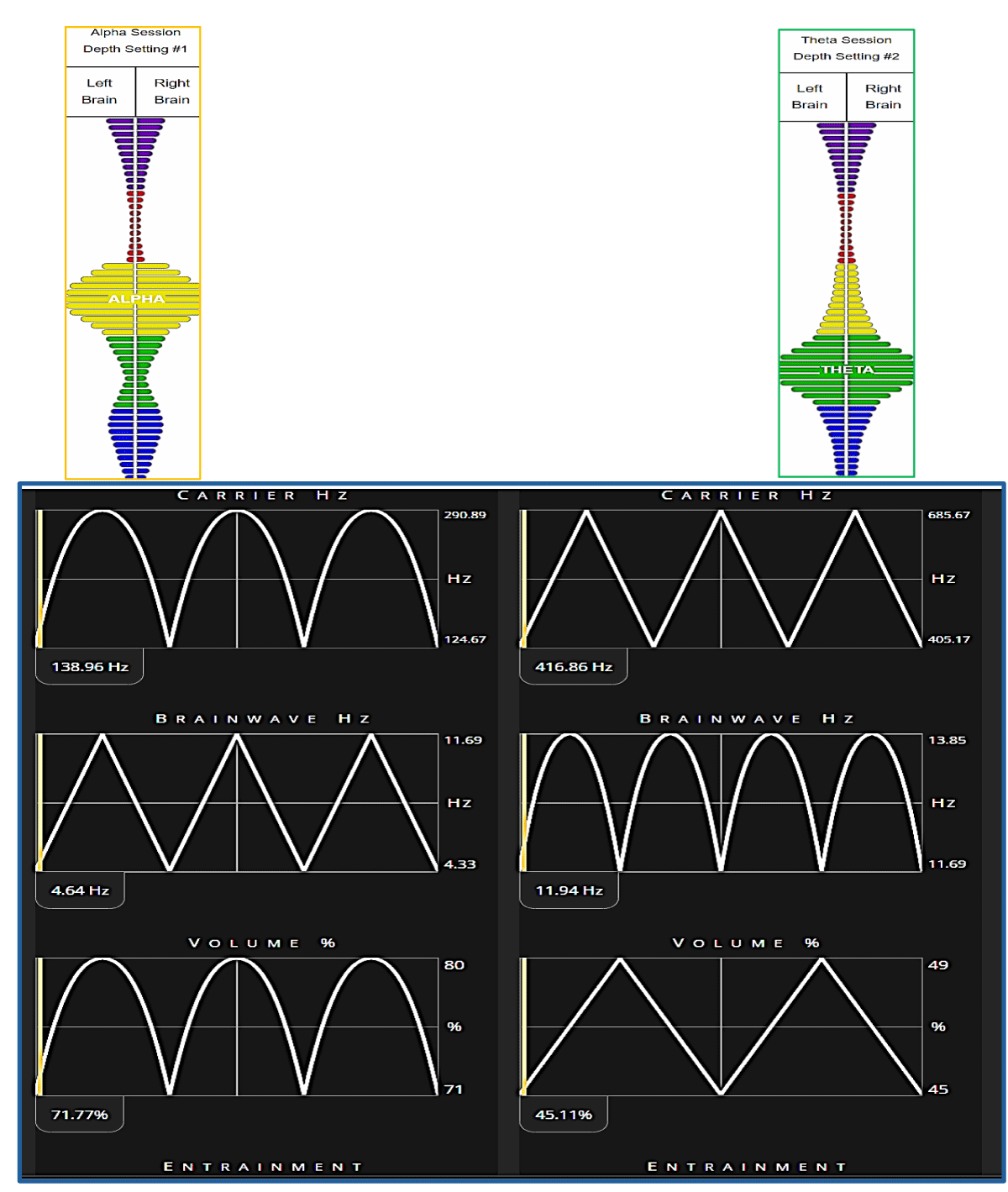
| Brain wave entrainment | 1 and II | 5.2.1 Alpha theta audio entrainment | 21 days for each stage 1 and stage 3 | For alpha and lower beta stage |
| Cerebration Techniques | II and III | 5.3.1 Cognoscere | 51 days twice a week | Emotional Intelligence and Cognitive Intelligence |
| 5.3.2 Emovere | 33 days stage 2 once a week/stage 3 twice a week | |||
| Bibliotherapy | I, II, III | 5.4.1 Books/articles reading | 1 day/week | Wisdom and Knowledge |
| Physical Body Movement | I, II, III | 5.4.1 Yoga/Exercise | SOS | Physical and Physiological health |
| Spiritual Practices | 1I and II | 5.4.1 Prayer and Gratitude | Daily Practice for 5-10 minutes | Confidence and motivation |
| Diet Protocols | 2.5 and III | 5.4.1 Light food/Intermittent fasting for 14:10 | SOS | Physiological health to keep a healthy mind, body, and behavior |
| Mindfulness interventions | II and III | 5.4.2 Muse Headband | Once a week for Stage 1/ Twice a week for Stage 2 and thrice a week for Stage 3 | Mindful relaxation and cognitive potentiation |
| *CURE Plan Stages: Three stages 1, 2, and 3 of 33 days each | ||||
Cognitive training and cognitive rehabilitation
Cognifit cognitive exercises/tasks: Cognifit cab: Computer-based cognitive training: Evidence supports the effectiveness and durability of cognitive training interventions in improving targeted cognitive abilities [51]. Cognitive training (CT) refers to the use of interventions aimed at improving cognitive domains through repeated practice of theoretically driven skills and strategies [23]. CT exercise aims to target one or two specific domains in an adaptive manner with a possibility of transfer effects whereby performance in other untrained cognitive domains is also improved [23]. Computerized CT (CCT) uses computers for the delivery of the intervention and differs from traditional CT, which usually incorporates face-to-face contact with a professional and paper-and-pencil paradigm in terms of advantages viz; cost-effectiveness, increased accessibility, and ability to customize the content and difficulty of the training [23,52]. Various evidence concluded that self-administered Computerized Cognitive Training based on gamified cognitive tasks could be an effective way to ameliorate cognitive dysfunction [29].
After the initial screening in Plan CARE was completed, the digital platform automatically and consecutively assigned the client to the training phase where the client was asked to complete short, gamified sessions of around 10 min each, consisting of a variety of tasks specifically designed for the training of different cognitive skills. Each training session included two different gamified cognitive tasks selected from a pool of 12 activities. Each training program was tailored to the individuals’ specific cognitive strengths and weaknesses detected in the CAB by a patented Individualized Training System™ (ITS) software that automatically chooses the activities and difficulty levels for each person in every session. A description of the 12 individual tasks used in the computerized cognitive training is presented as Supplementary Material. Client FP-33CV was asked to complete training every alternate day for a period of 12 weeks. After the 12 weeks of training, client FP-33 CV was again assessed and completed the CAB to see the difference in the cognitive skills score and improvement if any since the beginning of the Cognitome Program and at the end of the Cognitome Program.
Cognitive exercises/Tasks: Manual/Pen-paper-based: Pen paper-based/Manual cognitive exercises and tasks focused on improving the cognitive domains like memory, sustained attention, coordination, focused attention, perception, inhibitory control, cognitive flexibility/updating, reaction time, processing speed, etc. were assigned following the worksheet protocols by Happy Neuron Pro (https://www.happyneuronpro.com/en/) for manual cognitive training. The task was allotted a time frame to be completed starting from 10 mins eventually reducing to 3 mins in the successive sessions under the stop-watch timer. Time-based qualitative assessment was done every week for each task.
Audio-visual entrainment: AV entrainment like brain wave entrainment is a nonlinear, plastic process that utilizes physiological processes to modulate neurons [53], used for sleep, stress reduction, and improved concentration [54]. The brainwave entrainment hypothesis, states that external stimulation at a particular frequency synchronizes the brain’s electrocortical activity to oscillate at the same frequency opening avenues for research on the effects of binaural beat stimulation on cognitive and affective states [55]. Evidences suggest that studies, conducted in applied fields, usually refer to neuroscientific research demonstrating that binaural beats elicit systematic changes in EEG parameters [55]. When the subject is presented with two acoustic signals of slightly different frequencies separately to each ear, and then the percept of a third tone located in the head, or between the ears, oscillating at the difference of the two frequencies arises and the percept of this third tone is described as a psychoacoustic phenomenon ‘binaural beat [56]. When, for example, a tone with a frequency of 400 Hz is presented to the right ear and a second tone with a frequency of 420 Hz is presented to the left ear simultaneously, a binaural beat of 20 Hz will occur [55]. Binaural beat, a perceptual phenomenon without an external source, makes it of interest for research on sound perception and acoustic processing [57].
Equisync: EquiSync® sound technology guides you into different mind states (and various states of meditation) via brainwave entrainment. EquiSync excludes beta brainwaves and entrains only those responsible for the most beneficial states of consciousness: alpha, theta, delta, and gamma. With a focus on the mega-powerful Alpha, Theta, Delta, and Gamma brainwave frequencies, EquiSync is designed to mirror the natural brainwave state of an advanced meditator to tap into much deeper, much more pleasurable, and much higher quality states of meditation to experience the deepest, most highly beneficial states of consciousness with amazing results. Equisync Elements and Classic were used for the acoustic brainwave entrainment to train alpha and theta brain wave frequencies (https://www.eocinstitute.org).
Alpha brain wave frequency (7-13Hz) is seen at the beginning of meditation when mind chatter slows down. It is great for learning, the flow of creative Ideas, the reversal of negative habits, fears, phobias, and awake calm, and peaceful state, Alpha frequency entrainment helps in better focus, relaxation, and release of serotonin and endorphins and is excellent for reversal of anxiety, depression, stress, panic and boosting brain-mind power, happiness and confidence [58-60]. Theta brain wave frequency (4-7 Hz) is seen at the state of deep meditation, stage of sleep, vivid dream Imagery, connectedness, creativity, insight, intuition, and inspiration. Theta frequency entrainment helps in attaining better sleep, lowering cortisol, improving emotional Intelligence, and lowering pain [61].
Cerebration techniques of the cure plan of the cognitome program:
Cognoscere: Cognitive tasks like comprehension exercises for a book paragraph, Mathematical calculations, writing an excerpt out of an article as suggested by the CURE PLAN, etc. have been employed for manual cognitive training. The task was allotted a time frame to be completed starting from 10 mins eventually reducing to 3 mins in the successive sessions under the stop-watch timer. Time-based and qualitative assessment was done after every week for each task.
Emovere: Tasks related to suppressed emotions and positive and negative feelings were assigned. The client was asked to discuss, think, and then make an art piece or write a poetry/article on disturbing emotions. The client was also asked to write affirmations as suggested per the CURE PLAN a certain number of repetitions and practice gratitude both verbally and in writing.
Holistic approaches: Bibliotherapy, Mindfulness-based interventions including a ‘TEAM’ effort (Thoughtful eating, Exercise, Awareness of breathing, and Meditation) were also employed as a part of the Plan CURE of the Cognitome Program. These holistic approaches were tailored as per the issues of the client and advised and designed accordingly.
Muse meditation protocol: Meditative protocol was suggested using the MUSE 2 meditation device and meditation application. MUSE 2 (InteraXon Inc, Ontario, Canada) is a clinical-grade multi-sensor EEG headband device designed to interact with a mobile device (a smartphone or tablet) (https://choosemuse.com) with real-time feedback on what is happening with one’s brain activity while one is meditating and helps one learn quickly [62]. Muse’s finely calibrated EEG sensors - 2 on the forehead (FP1, FP2), 2 behind the ears (T9, T10), and a reference sensor (FPz) - detect and measure the activity of your brain. Its PPG sensor measures your heart rate, while an accelerometer and gyroscope measure your breath rhythm and body movement. Muse 2 senses what is going on in your mind, in the form of your brainwaves, and guides you to control them. It does this by using advanced signal processing to convert your brainwaves into the sounds of weather. When one’s mind is calm and settled, hear peaceful weather. As focus drifts, one begins to hear stormy weather, serving as a cue to bring one’s attention back on track. Each meditation session can vary in length for the participant and can be set from 5 minutes to 45 minutes per session. Mindfulness-based interventions and meditation have been shown to reduce stress, and anxiety, and improve focus, cognitive flexibility, and productivity [63,64]. For each mediation session for Client FP-33CV, mind meditation, guided meditation, Body and Breath Meditation, and heart meditation were suggested as available in the Muse app. Each session started from 5 mins for the initial weeks and progressed up to 30 mins in the subsequent weeks.
Following the Cognitome program for approximately 4 months - an improvement in the cognitive profile/abilities was observed along with a prominent reduction in the symptoms of anxiety, and depression, lesser frequency of headaches, and better sleep routine, thereby adding to better physical/ psychological well-being of the client FP-33CV. This is indicated by the better test scores, continuous interviewing of the client, as well as the client’s self-evaluation done using the client exit form at the end of the Cognitome program. Data analysis was done by evaluating the difference in qualitative subjective scores between the initial and final assessments as the main outcome measure for evaluating the improvement in the subjective symptoms of anxiety/depression as well as for the cognitive abilities/skills. The scores before and after the program are inferred as an increase (+++;++,+)/decrease(---/--/-) of the domain assessed and total average score of all the cognitive domains assessed.
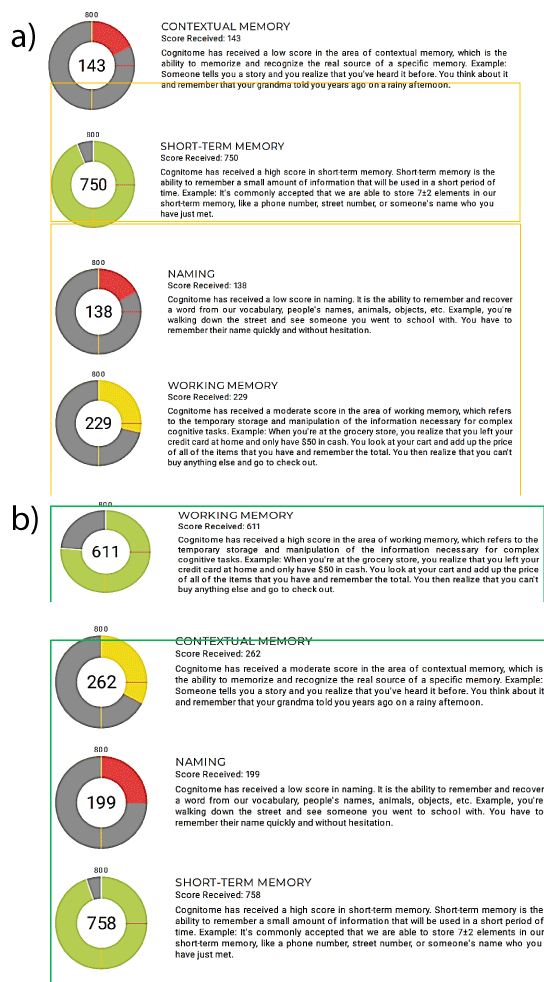
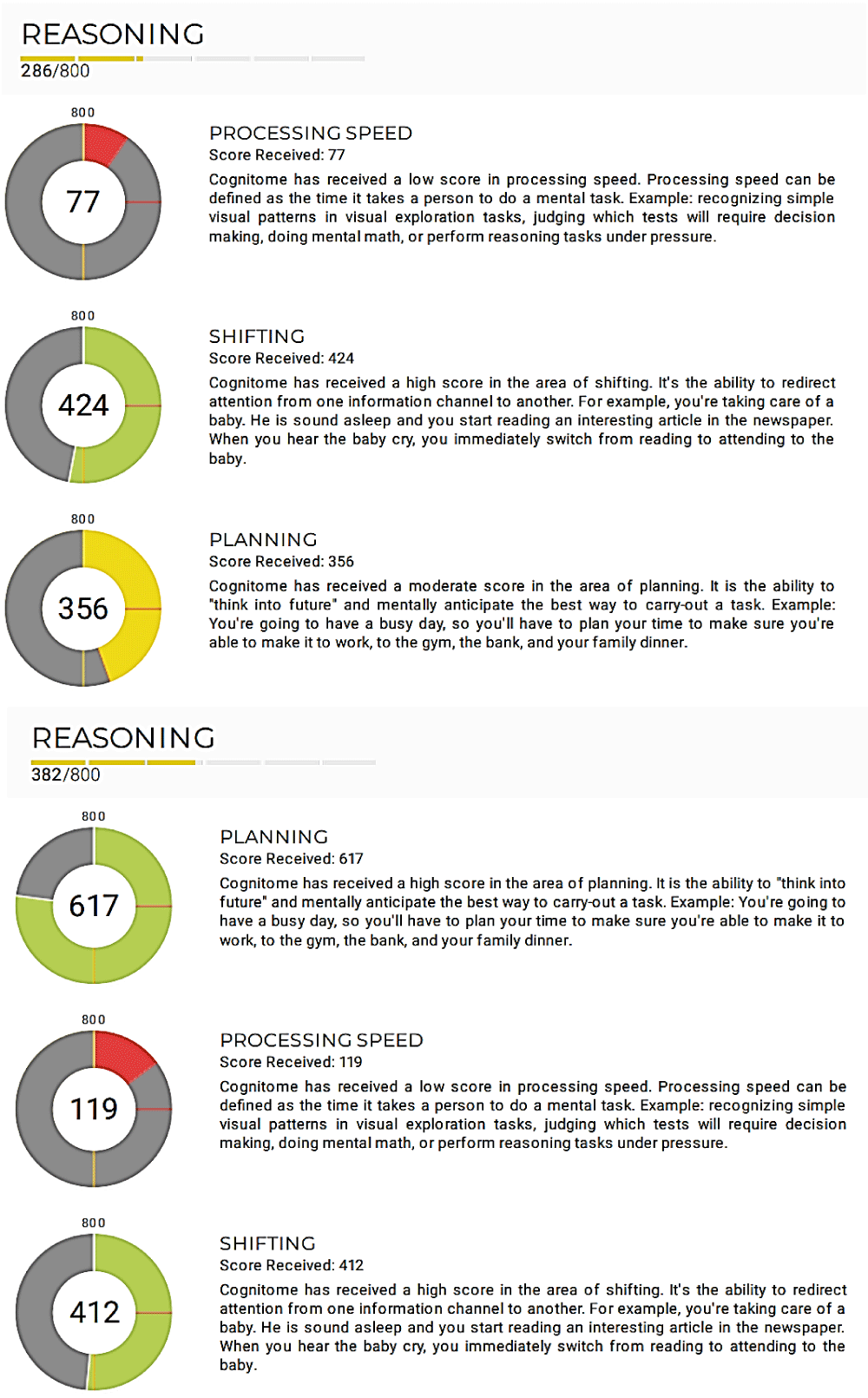
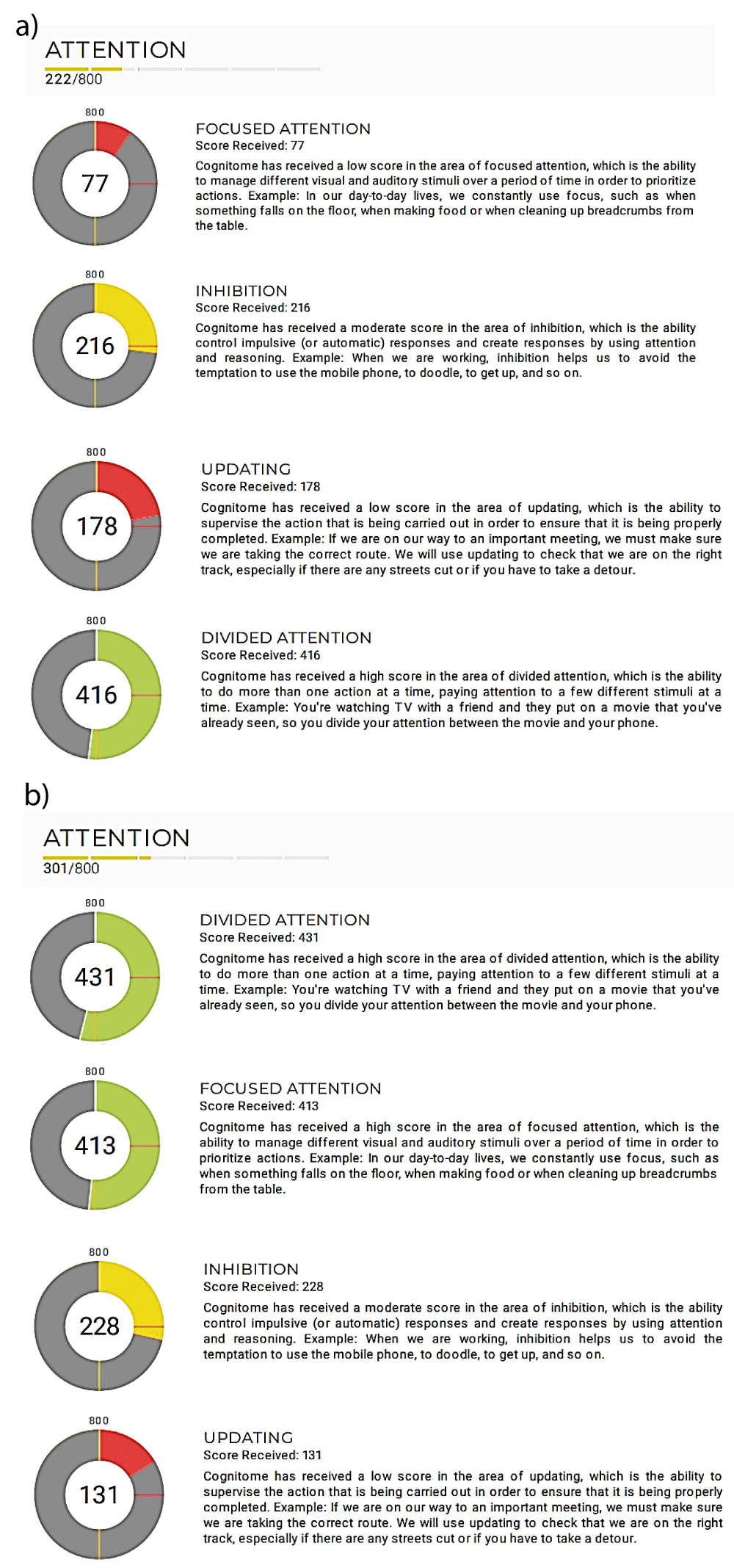
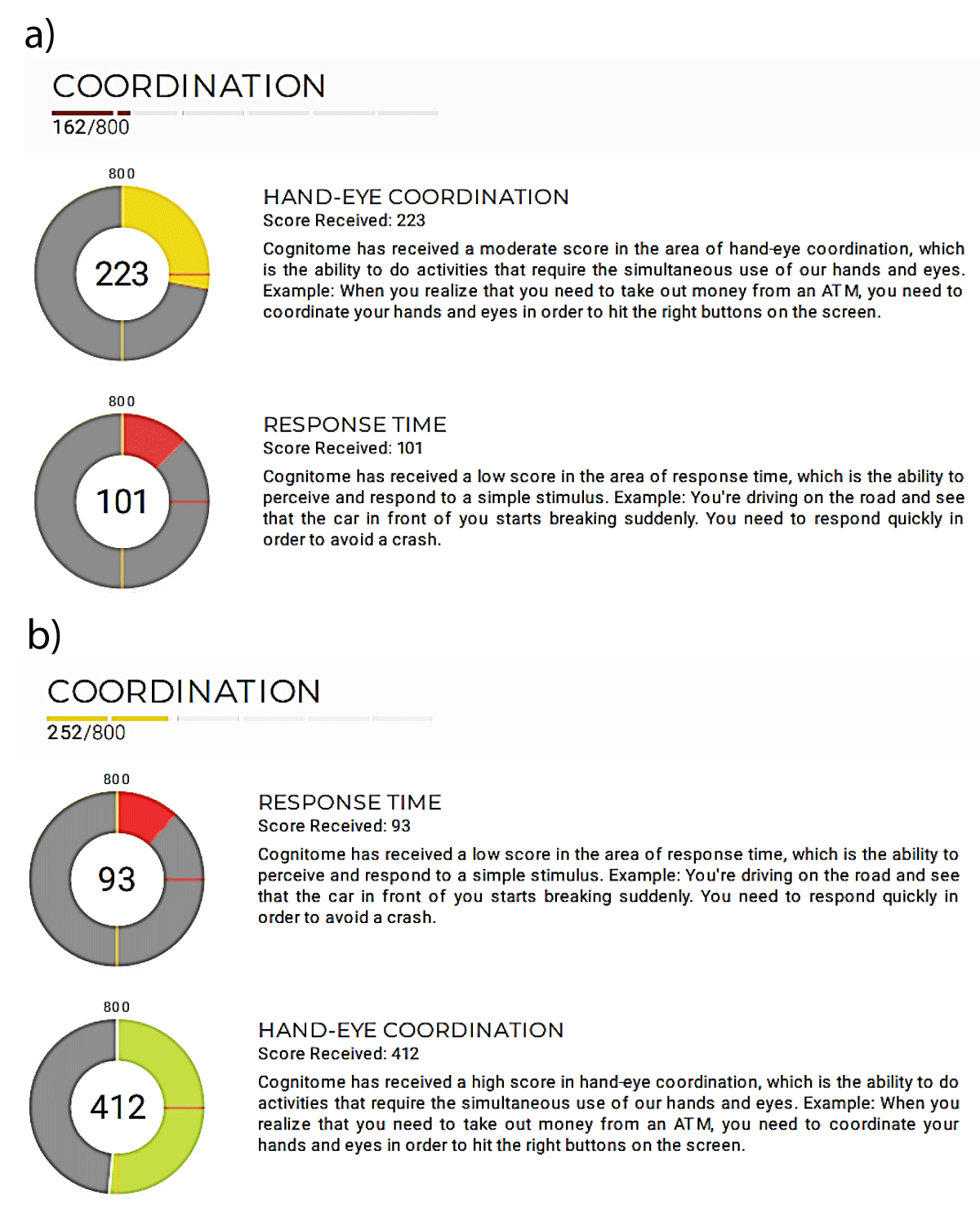
The scores indicated that following the Cognitome program for 3 months and 15 days- an improvement in the cognitive profile/abilities was seen along with a prominent reduction in the symptoms of anxiety, and depression at the conclusion of the program. Though scores of the spirituality index scale and centrality of religiosity have shown a consistent trend as FP-33CV has clearly mentioned during the interview and in the C-IES about her discipline and high inclination towards spirituality. Subjectively, a lesser frequency of headaches and a better sleep routine were observed as stated by the client adding to her better physical/ psychological well-being. Besides, at the conclusion of the Cognitome program client, FP-33CV evaluated herself by answering the questionnaire as mentioned in the Client Exit Form of the Cognitome Program. The detailed scores of various tests/assessments done both at the beginning and at the end of the Cognitome program are charted and mentioned in Tables 1-4 and Figures 1a-c – 10a-b.
| Table 3: Average scores of cognitive skills before/after cognitome program. | |||
| Cognitive Domains | Cognifit cab-pro before cognitome program (overall average score out of 800) | Cognifitcab-proafter cognitome program (overall average score out of 800) | Inference (overall) |
| Memory | 315 | 457.5 | +++ improvement |
| Reasoning | 282 | 386 | ++ improvement |
| Attention | 222 | 301 | + improvement |
| Coordination | 162 | 252 | ++ improvement |
| Perception | 185 | 270 | + improvement |
| Total Average Score | 233.2 | 336.8 | ++ improvement |
| *** (+++):After Cognitome program score is high indicating Improved cognitive function/skill **(++): After Cognitome program score is good indicating better cognitive function/skill *(+): After Cognitome program score is fair indicating a positive change in cognitive function/skill ***(---): After Cognitome program score is lesser indicating a decrease in the cognitive function/skill **(--/-): After Cognitome program score is less indicating a decrease in the cognitive function/skill |
|||
| Table 4: Scores of sub-domains of the cognitive skills before/after cognitome program. | ||||
| Cognitive Domain | Sub-domain | Score out of 800 Before Cognitome Program | Score out of 800 After Cognitome Program | Inference |
| Memory | Naming | 138 | 199 | + Improved |
| Contextual memory | 143 | 262 | + Improved | |
| Working memory | 229 | 611 | +++Improved | |
| Short-term memory | 750 | 758 | Same: High score (very good) | |
| Attention | Divided attention | 416 | 431 | Same: good |
| Focused attention | 77 | 413 | ++improved | |
| Updating | 178 | 131 | (-) Decreased | |
| Inhibition | 216 | 228 | Same: fair | |
| Reasoning | Processing speed | 77 | 119 | (+) better |
| Planning | 356 | 617 | (+++) improved | |
| Shifting | 424 | 412 | Same: good | |
| Coordination | Response time | 223 | 93 | (---) Decreased |
| Hand-eye coordination | 101 | 412 | (++) improved | |
| Perception | Auditory perception | 173 | 296 | (+) Fair |
| Estimation | 08 | 08 | No change: Poor | |
| Recognition | 132 | 618 | (+++) improved | |
| Spatial perception | 676 | 202 | (---) Decreased | |
| Visual scanning | 26 | 239 | (++) Improved | |
| Visual perception | 97 | 256 | (++) Improved | |
| *** (+++):After Cognitome program score is high indicating Improved cognitive function/skill **(++): After Cognitome program score is good indicating better cognitive function/skill *(+): After Cognitome program score is fair indicating a positive change in cognitive function/skill ***(---): After Cognitome program score is lesser indicating a decrease in the cognitive function/skill **(--/-): After Cognitome program score is less indicating a decrease in the cognitive function/skill |
||||
Figure 1: Brain hemispheric dominance tests. a) Before cognitome program; b) After cognitome program, c) Brain Hemispheric Difference
Figure 2: Neurobehavioral cognitive profiling: Cognistat Cas Pro(II). A) Before cure plan. b): After cure plan.
Figure 3: Alpha /theta brain wave entrainment: source-equisync, eco institute.
Figure 4: Plan care: Well-Being Indicators. a) Before Cognitome Program, b) After Cognitome Program.
Figure 5: Plan care: Cognitive Profile. a) Before cognitome program, b) After cognitome program..
Figure 6: a): Cognifit CAB-PRO memory profile: Before cognitome program. b): Cognifit CAB-PRO memory profile: after cognitome program.
Figure 7: Cognifit CAB-PRO reasoning profile: a) before and b) after cognitome program.
Figure 8: a): Cognifit CAB-PRO attention profile: before cognitome program. b): Cognifit CAB-PRO attention profile: after cognitome program.
Figure 9: a) Cognifit CAB-PRO attention profile: before cognitome program. b): Cognifit CAB-PRO attention profile: after cognitome program.
Figure 10: a): Cognifit CAB-PRO Perception Profile: Before Cognitome Program.
The human brain is a vastly adaptable neuroplastic organ with trillions of neural connections. Being highly neuroplastic in nature it has immense potential to modify, change, and adapt both structurally and functionally [28,65]. Evidence suggests that mechanisms of neural plasticity (neurogenesis, synaptogenesis, dendritic arborization, and network re-organization) support cognitive plasticity (patterns of cognitive behavior and dependence on executive control), and both get stimulated by learning and novelty, education and training, dietary manipulations, aerobic exercise [20]. To enhance this interactive process and trigger plastic changes- cognitive integrity (preserved cognitive ability) and brain integrity (preserved brain structure) environmental enrichment and exposure to novel experiences, training, and learning are important triggers for improved cognitive performance and increased brain weight and cortical plasticity [20,66,67]. Therefore, we can rewire our brain by creating entirely new neural pathways by exploiting its neuroplastic nature. This presents tremendous opportunities for learning new skills and behavior and unlearning patterns of thinking blocking personal and professional growth. A rewired brain functions a bit differently from how it previously functioned due to the resultant novel connections that might induce cortical remapping, circuit, and network changes by learning a new task, environmental influences, repetition, and mental exercises [28,65]. As discussed, earlier use of supportive therapies, talk therapies viz; guidance and counseling and use of pharmacological drugs for the treatment of anxiety and depression have their own limitations and pitfalls. Considering these limitations, it is recommended to use various cognitive training strategies aiming at cognitive remediation, and cognitive rehabilitation are explicit interventional approaches designed to address difficulties with cognitive functioning [18]. Evidence shows that Computerized Cognitive Training programs are a feasible option for individuals with MCI, with equal or better adherence rates when compared with traditional CT [23]. Besides, evidence also suggests that Mindfulness-based interventions can assist in observing and comprehending emotions, emotional responses, and emotional awareness improving one’s reasoning abilities and cognitive flexibility [26,63]. Further, evidence suggests that Auditory beat stimulation [68] or Binaural /Monoaural beats [55,56] may be a promising new tool for the manipulation of cognitive processes and the modulation of mood states. Studies have shown that cognitive stimulation programs minimally aiming at a period of 12 weeks (includes computer-based cognitive exercises and pen/paper-based cognitive tasks) have a beneficial effect on cognitive performance, anxiety, depression, and mild cognitive impairment [29]. Evidence suggests that Cognitive training programs have also exhibited improvements not only in the mental/cognitive domains but also in overall quality of life, encompassing betterment in emotional control, social function, vitality, and mental health, as well as in physical health [51].
The “Cognitome Program” is a type of cognitive remediation program, developed as an outcome of years of research and studies blending the elements from neuroscience and neuropsychology to help everyone tap the vast reservoir of resources available in the brain by exploiting the concept of functional and structural neuroplasticity. It is an individual and age-specific, customized therapeutic plan based on needful assessments, detailed evaluation, and careful analysis of results- a stepwise process to have a complete understanding of the mental and physical condition of the client, followed by devising the most suitable course of action for the client. Subjects after the Cognitome Program have experienced unparalleled cognitive skills enhancement and improvement of cognitive functions along with better emotional intelligence, and enhanced creativity. Specially devised to boost memory retention, and attention, enhance critical thinking, and creative thinking, and optimize overall cognitive functions, the Cognitome program offers a transformative journey tailored to one’s unique cognitive needs as exhibited by this case study of the client FP-33CV.
Emerging evidence for cognitive dysfunction in depressive and anxiety disorders is associated with serious and long-lasting psychosocial, and occupational difficulties. GAD and related depression can be chronic, impairing, and debilitating not only for psychological well-being but also for cognitive abilities/functions. Detailed neuropsychological examination includes an interview of the patient’s background and present situation, a behavioral observation, and neuropsychological tests charting the required information to be used in the patient’s treatment planning, evaluating the efficacy of the treatment plan as well as in individual-specific differential diagnosis. Following these steps, The Cognitome Program, a structured, neuroscientific cognitive rehabilitation protocol guided by the concept of neuroplasticity was used as a therapeutic interventional tool for the case FP-33CV. The client has clearly exhibited significant improvement in cognitive skill/functions, ameliorated the symptoms of anxiety and related depression with lesser frequency of headaches, and attained a better sleep routine thereby not only improvising cognitive functions like memory, processing speed, focus/attention but also their overall well-being and quality of life proving the efficaciousness of the holistic neuroscientific approach of the Cognitome Program.
- Grillon C, Robinson OJ, Cornwell B, Ernst M. Modeling anxiety in healthy humans: a key intermediate bridge between basic and clinical sciences. Neuropsychopharmacology. 2019 Nov;44(12):1999-2010. doi: 10.1038/s41386-019-0445-1. Epub 2019 Jun 21. PMID: 31226707; PMCID: PMC6897969.
- Castaneda AE, Tuulio-Henriksson A, Marttunen M, Suvisaari J, Lönnqvist J. A review on cognitive impairments in depressive and anxiety disorders with a focus on young adults. J Affect Disord. 2008 Feb;106(1-2):1-27. doi: 10.1016/j.jad.2007.06.006. Epub 2007 Aug 20. PMID: 17707915.
- Chisholm D, Sweeny K, Sheehan P, Rasmussen B, Smit F. Scaling-up treatment of depression and anxiety: a global return on investment analysis. Lancet Psychiatry. 2016 May;3(5):415-24. doi: 10.1016/S2215-0366(16)30024-4.
- LeDoux JE, Pine DS. Using neuroscience to help understand fear and anxiety: a two-system framework. Am J Psychiatry. 2016 Oct 1;173(10):1083-93. doi: 10.1176/appi.ajp.2016.16030353..
- Gkintoni E, Ortiz PS. Neuropsychology of Generalized Anxiety Disorder in Clinical Setting: A Systematic Evaluation. Healthcare (Basel). 2023 Aug 31;11(17):2446. doi: 10.3390/healthcare11172446. PMID: 37685479; PMCID: PMC10486954.
- Lukasik KM, Waris O, Soveri A, Lehtonen M, Laine M. The Relationship of Anxiety and Stress With Working Memory Performance in a Large Non-depressed Sample. Front Psychol. 2019 Jan 23;10:4. doi: 10.3389/fpsyg.2019.00004. PMID: 30728790; PMCID: PMC6351483.
- Balderston NL, Flook E, Hsiung A, Liu J, Thongarong A, Stahl S, Makhoul W, Sheline Y, Ernst M, Grillon C. Patients with anxiety disorders rely on bilateral dlPFC activation during verbal working memory. Soc Cogn Affect Neurosci. 2020 Dec 24;15(12):1288-1298. doi: 10.1093/scan/nsaa146. PMID: 33150947; PMCID: PMC7759210.
- Fitzgerald JM, Phan KL, Kennedy AE, Shankman SA, Langenecker SA, Klumpp H. Prefrontal and amygdala engagement during emotional reactivity and regulation in generalized anxiety disorder. J Affect Disord. 2017 Aug 15;218:398-406. doi: 10.1016/j.jad.2017.05.013. Epub 2017 May 7. PMID: 28501740; PMCID: PMC6608590.
- Perini G, Cotta Ramusino M, Sinforiani E, Bernini S, Petrachi R, Costa A. Cognitive impairment in depression: recent advances and novel treatments. Neuropsychiatr Dis Treat. 2019 May 10;15:1249-1258. doi: 10.2147/NDT.S199746. PMID: 31190831; PMCID: PMC6520478.
- Lam RW, Kennedy SH, McIntyre RS, Khullar A. Cognitive Dysfunction in Major Depressive Disorder: Effects on Psychosocial Functioning and Implications for Treatment. Can J Psychiatry. 2014 Dec;59(12):649-654. doi: 10.1177/070674371405901206.
- Haimov I, Hanuka E, Horowitz Y. Chronic insomnia and cognitive functioning among older adults. Behav Sleep Med. 2008;6(1):32-54. doi: 10.1080/15402000701796080. PMID: 18412036.
- Dominguez LJ, Veronese N, Vernuccio L, Catanese G, Inzerillo F, Salemi G, Barbagallo M. Nutrition, Physical Activity, and Other Lifestyle Factors in the Prevention of Cognitive Decline and Dementia. Nutrients. 2021 Nov 15;13(11):4080. doi: 10.3390/nu13114080. PMID: 34836334; PMCID: PMC8624903.
- Beddington J, Cooper CL, Field J, Goswami U, Huppert FA, Jenkins R, Jones HS, Kirkwood TB, Sahakian BJ, Thomas SM. The mental wealth of nations. Nature. 2008 Oct 23;455(7216):1057-60. doi: 10.1038/4551057a. PMID: 18948946.
- Robinson OJ, Vytal K, Cornwell BR, Grillon C. The impact of anxiety upon cognition: perspectives from human threat of shock studies. Front Hum Neurosci. 2013 May 17;7:203. doi: 10.3389/fnhum.2013.00203. PMID: 23730279; PMCID: PMC3656338.
- Koen N, Stein DJ. Pharmacotherapy of anxiety disorders: a critical review. Dialogues Clin Neurosci. 2011;13(4):423-37. doi: 10.31887/DCNS.2011.13.4/nkoen. PMID: 22275848; PMCID: PMC3263390.
- Zoellner LA, Foa EB. Applying Research Domain Criteria (RDoC) to the study of fear and anxiety: A critical comment. Psychophysiology. 2016 Mar;53(3):332-5. doi: 10.1111/psyp.12588. PMID: 26877122.
- Orgeta V, Leung P, Del-Pino-Casado R, Qazi A, Orrell M, Spector AE, Methley AM. Psychological treatments for depression and anxiety in dementia and mild cognitive impairment. Cochrane Database Syst Rev. 2022 Apr 25;4(4):CD009125. doi: 10.1002/14651858.CD009125.pub3. PMID: 35466396; PMCID: PMC9035877.
- Bahar-Fuchs A, Clare L, Woods B. Cognitive training and cognitive rehabilitation for mild to moderate Alzheimer's disease and vascular dementia. Cochrane Database Syst Rev. 2013 Jun 5;2013(6):CD003260. doi: 10.1002/14651858.CD003260.pub2. PMID: 23740535; PMCID: PMC7144738.
- Barman A, Chatterjee A, Bhide R. Cognitive Impairment and Rehabilitation Strategies After Traumatic Brain Injury. Indian J Psychol Med. 2016 May-Jun;38(3):172-81. doi: 10.4103/0253-7176.183086. PMID: 27335510; PMCID: PMC4904751.
- Greenwood PM, Parasuraman R. Neuronal and cognitive plasticity: a neurocognitive framework for ameliorating cognitive aging. Front Aging Neurosci. 2010 Nov 29;2:150. doi: 10.3389/fnagi.2010.00150. PMID: 21151819; PMCID: PMC2999838.
- Frohlich F, Riddle J, Ugen G, Lersch F. Brainwave entrainment for the treatment of chronic pain. Br J Pain. 2020 Aug;14(3):161-170.
- Yadav GS, Cidral-Filho FJ, Iyer RB. Using Heartfulness Meditation and Brainwave Entrainment to Improve Teenage Mental Wellbeing. Front Psychol. 2021 Oct 15;12:742892. doi: 10.3389/fpsyg.2021.742892. PMID: 34721219; PMCID: PMC8554296.
- Zhang H, Huntley J, Bhome R, Holmes B, Cahill J, Gould RL, Wang H, Yu X, Howard R. Effect of computerised cognitive training on cognitive outcomes in mild cognitive impairment: a systematic review and meta-analysis. BMJ Open. 2019 Aug 18;9(8):e027062. doi: 10.1136/bmjopen-2018-027062. PMID: 31427316; PMCID: PMC6701629.
- Gomez-Soria I, Peralta-Marrupe P, Plo F. Cognitive stimulation program in mild cognitive impairment A randomized controlled trial. Dement Neuropsychol. 2020 Apr-Jun;14(2):110-117. doi: 10.1590/1980-57642020dn14-020003. PMID: 32595879; PMCID: PMC7304274.
- Asensio D, Duñabeitia JA. The necessary, albeit belated, transition to computerized cognitive assessment. Front Psychol. 2023 Apr 24;14:1160554. doi: 10.3389/fpsyg.2023.1160554. PMID: 37168430; PMCID: PMC10165007.
- Wilson KG, Sandoz EK. Mindfulness, values, and the therapeutic relationship in acceptance and commitment therapy. In: Hick S, Bein T, editors. Mindfulness and the therapeutic relationship. Guilford Press; 2008.
- Garner AR, Stuart GL. Integrating Mindfulness and Acceptance Into Traditional Cognitive Behavioral Therapy During the COVID-19 Pandemic: A Case Study of an Adult Man With Generalized Anxiety Disorder. Clin Case Stud. 2023 Apr;22(2):120-137. doi: 10.1177/15346501221123568. Epub 2022 Aug 23. PMID: 38603362; PMCID: PMC9403529.
- Berns C, Brüchle W, Scho S, Schneefeld J, Schneider U, Rosenkranz K. Intensity dependent effect of cognitive training on motor cortical plasticity and cognitive performance in humans. Exp Brain Res. 2020 Dec;238(12):2805-2818. doi: 10.1007/s00221-020-05933-5. Epub 2020 Oct 6. PMID: 33025030; PMCID: PMC7644474.
- Duñabeitia JA, Mera F, Baro Ó, Jadad-Garcia T, Jadad AR. Personalized Computerized Training for Cognitive Dysfunction after COVID-19: A Before-and-After Feasibility Pilot Study. Int J Environ Res Public Health. 2023 Feb 10;20(4):3100. doi: 10.3390/ijerph20043100. PMID: 36833793; PMCID: PMC9966004.
- Hofmann SG, Sawyer AT, Witt AA, Oh D. The effect of mindfulness-based therapy on anxiety and depression: A meta-analytic review. J Consult Clin Psychol. 2010 Apr;78(2):169-83. doi: 10.1037/a0018555. PMID: 20350028; PMCID: PMC2848393.
- Hamilton M. Development of a rating scale for primary depressive illness. Br J Soc Clin Psychol. 1967 Dec;6(4):278-96. doi: 10.1111/j.2044-8260.1967.tb00530.x. PMID: 6080235.
- Beck AT, Epstein N, Brown G, Steer RA. An inventory for measuring clinical anxiety: psychometric properties. J Consult Clin Psychol. 1988 Dec;56(6):893-7. doi: 10.1037//0022-006x.56.6.893. PMID: 3204199.
- Spitzer RL, Kroenke K, Williams JB, Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006 May 22;166(10):1092-7. doi: 10.1001/archinte.166.10.1092. PMID: 16717171.
- Hamilton M. The assessment of anxiety states by rating. Br. J. Med. Psychol. 1959; 32:50–55. doi: 10.1111/j.2044-8341. 1959.tb00467.
- BECK AT, WARD CH, MENDELSON M, MOCK J, ERBAUGH J. An inventory for measuring depression. Arch Gen Psychiatry. 1961 Jun;4:561-71. doi: 10.1001/archpsyc.1961.01710120031004. PMID: 13688369.
- Henry JD, Crawford JR. The short-form version of the Depression Anxiety Stress Scales (DASS-21): construct validity and normative data in a large non-clinical sample. Br J Clin Psychol. 2005 Jun;44(Pt 2):227-39. doi: 10.1348/014466505X29657. PMID: 16004657.
- Lovibond SH, Lovibond PF. Manual for the Depression Anxiety Stress Scales. 2nd ed. Sydney: Psychology Foundation; 1995.
- Burckhardt CS, Woods SL, Schultz AA, Ziebarth DM. Quality of life of adults with chronic illness: a psychometric study. Res Nurs Health. 1989 Dec;12(6):347-54. doi: 10.1002/nur.4770120604. PMID: 2602575.
- Flanagan JC. Measurement of quality of life: current state of the art. Arch Phys Med Rehabil. 1982 Feb;63(2):56-9. PMID: 6460487.
- Daaleman TP, Frey BB. The Spirituality Index of Well-Being: A New Instrument for Health-Related Quality of Life Research. Ann Fam Med. 2004 Sep-Oct;2(5):499-503.
- Huber S. Are religious beliefs relevant in daily life? In: Streib H, editor. Religion Inside and Outside Traditional Institutions. Leiden: Brill Academic Publishers; 2007; 211-230.
- Araújo P, Gomes S, Vidal DG, Sousa HFPE, Dinis MAP, Leite Â. Preliminary Validation Study of the Intrinsic Religious Motivation Scale and the Centrality of Religiosity Scale for the Portuguese Population. Eur J Investig Health Psychol Educ. 2021 Aug 18;11(3):908-922. doi: 10.3390/ejihpe11030067. PMID: 34563080; PMCID: PMC8544200.
- Folstein M, Folstein SE, McHugh PR. "Mini-Mental State": a practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975 Nov;12(3):189-198.
- Nasreddine ZS, Phillips NA, Bédirian V, Charbonneau S, Whitehead V, Collin I, Cummings JL, Chertkow H. The Montreal Cognitive Assessment, MoCA: a brief screening tool for mild cognitive impairment. J Am Geriatr Soc. 2005 Apr;53(4):695-9. doi: 10.1111/j.1532-5415.2005.53221.x. Erratum in: J Am Geriatr Soc. 2019 Sep;67(9):1991. doi: 10.1111/jgs.15925. PMID: 15817019.
- Tariq SH, Tumosa N, Chibnall JT, Perry MH 3rd, Morley JE. Comparison of the Saint Louis University mental status examination and the mini-mental state examination for detecting dementia and mild neurocognitive disorder--a pilot study. Am J Geriatr Psychiatry. 2006 Nov;14(11):900-10. doi: 10.1097/01.JGP.0000221510.33817.86. PMID: 17068312.
- Broadbent DE, Cooper PF, FitzGerald P, Parkes KR. The Cognitive Failures Questionnaire (CFQ) and its correlates. Br J Clin Psychol. 1982 Feb;21(1):1-16. doi: 10.1111/j.2044-8260.1982.tb01421.x. PMID: 7126941.
- Rast P, Zimprich D, Van Boxtel M, Jolles J. Factor structure and measurement invariance of the cognitive failures questionnaire across the adult life span. Assessment. 2009 Jun;16(2):145-58. doi: 10.1177/1073191108324440. Epub 2008 Dec 9. PMID: 19066391.
- Jorgenson E. Development of the Open Hemispheric Brain Dominance Scale. 2015. Available from: http://openpsychometrics.org/tests/OHBDS/development/
- Yaneva A, Massaldjieva R, Mateva N. Initial Adaptation of the General Cognitive Assessment Battery by Cognifit™ for Bulgarian Older Adults. Exp Aging Res. 2022 Jul-Sep;48(4):336-350. doi: 10.1080/0361073X.2021.1981096. Epub 2021 Oct 3. PMID: 34605370.
- Buades-Sitjar F, Duñabeitia JA. Intelligence subcomponents and their relationship to general knowledge. J Cult Cogn Sci. 2022;6:343-355. doi: 10.1007/s41809-022-00113-z.
- Ball K, Berch DB, Helmers KF, Jobe JB, Leveck MD, Marsiske M, Morris JN, Rebok GW, Smith DM, Tennstedt SL, Unverzagt FW, Willis SL; Advanced Cognitive Training for Independent and Vital Elderly Study Group. Effects of cognitive training interventions with older adults: a randomized controlled trial. JAMA. 2002 Nov 13;288(18):2271-81. doi: 10.1001/jama.288.18.2271. PMID: 12425704; PMCID: PMC2916176.
- Gates N, Valenzuela M. Cognitive exercise and its role in cognitive function in older adults. Curr Psychiatry Rep. 2010 Feb;12(1):20-7. doi: 10.1007/s11920-009-0085-y. PMID: 20425306.
- Soutar P, Longo R. Doing Neurofeedback: An Introduction. 2011.
- Demos J. Getting Started with Neurofeedback. W. W. Norton & Company; 2005.
- Ingendoh RM, Posny ES, Heine A. Binaural beats to entrain the brain? A systematic review of the effects of binaural beat stimulation on brain oscillatory activity, and the implications for psychological research and intervention. PLoS One. 2023 May 19;18(5):e0286023. doi: 10.1371/journal.pone.0286023. PMID: 37205669; PMCID: PMC10198548.
- Orozco Perez HD, Dumas G, Lehmann A. Binaural Beats through the Auditory Pathway: From Brainstem to Connectivity Patterns. eNeuro. 2020 Mar 19;7(2):ENEURO.0232-19.2020. doi: 10.1523/ENEURO.0232-19.2020. PMID: 32066611; PMCID: PMC7082494.
- Ross B, Miyazaki T, Thompson J, Jamali S, Fujioka T. Human cortical responses to slow and fast binaural beats reveal multiple mechanisms of binaural hearing. J Neurophysiol. 2014 Oct 15;112(8):1871-84. doi: 10.1152/jn.00224.2014. Epub 2014 Jul 9. PMID: 25008412.
- Le Scouarnec RP, Poirier RM, Owens JE, Gauthier J, Taylor AG, Foresman PA. Use of binaural beat tapes for treatment of anxiety: a pilot study of tape preference and outcomes. Altern Ther Health Med. 2001 Jan;7(1):58-63. PMID: 11191043.
- Gupta A. Significance of alpha brainwaves in meditation examined from the study of binaural beats. In: International Conference on Signal Processing and Communication (ICSC); 2016. p. 484-489. doi: 10.1109/ICSPCom.2016.7980629.
- Seifi T. Cumulative effects of theta binaural beats on brain power and functional connectivity. Biomed Signal Process Control. 2018 Apr;42:242-252.
- Zampi DD. Efficacy of Theta-Binaural Beats for the Treatment of Chronic Pain. Northcentral University; 2015. ProQuest Dissertations Publishing 3670283.
- Ghosh K, Nanda S, Hurt RT, Schroeder DR, West CP, Fischer KM, Bauer BA, Fokken SC, Ganesh R, Hanson JL, Lindeen SA, Pruthi S, Croghan IT. Mindfulness Using a Wearable Brain Sensing Device for Health Care Professionals During a Pandemic: A Pilot Program. J Prim Care Community Health. 2023 Jan-Dec;14:21501319231162308. doi: 10.1177/21501319231162308. PMID: 36960553; PMCID: PMC10041582.
- Moore A, Malinowski P. Meditation, mindfulness and cognitive flexibility. Conscious Cogn. 2009 Mar;18(1):176-86. doi: 10.1016/j.concog.2008.12.008. Epub 2009 Jan 31. PMID: 19181542.
- Millstine DM, Bhagra A, Jenkins SM, Croghan IT, Stan DL, Boughey JC, Nguyen MT, Pruthi S. Use of a Wearable EEG Headband as a Meditation Device for Women With Newly Diagnosed Breast Cancer: A Randomized Controlled Trial. Integr Cancer Ther. 2019 Jan-Dec;18:1534735419878770. doi: 10.1177/1534735419878770. PMID: 31566031; PMCID: PMC6769228.
- Marusic U, Verghese J, Mahoney JR. Does Cognitive Training Improve Mobility, Enhance Cognition, and Promote Neural Activation? Front Aging Neurosci. 2022 May 23;14:845825. doi: 10.3389/fnagi.2022.845825. PMID: 35677205; PMCID: PMC9168002.
- Straube T, Korz V, Frey JU. Bidirectional modulation of long-term potentiation by novelty-exploration in rat dentate gyrus. Neurosci Lett. 2003 Jun 19;344(1):5-8. doi: 10.1016/s0304-3940(03)00349-5. PMID: 12781908.
- Grossman AW, Churchill JD, McKinney BC, Kodish IM, Otte SL, Greenough WT. Experience effects on brain development: possible contributions to psychopathology. J Child Psychol Psychiatry. 2003 Jan;44(1):33-63. doi: 10.1111/1469-7610.t01-1-00102. PMID: 12553412.
- Chaieb L, Wilpert EC, Reber TP, Fell J. Auditory beat stimulation and its effects on cognition and mood States. Front Psychiatry. 2015 May 12;6:70. doi: 10.3389/fpsyt.2015.00070. PMID: 26029120; PMCID: PMC4428073.
- Lezak MD. Neuropsychological Assessment. 4th ed. Oxford University Press; 2004.