More Information
Submitted: March 11, 2024 | Approved: April 16, 2024 | Published: April 17, 2024
How to cite this article: Machado S, dos Santos DF, De Martino Luppi A, Guimarães VV, da Silva AAL. Primary Diffuse Leptomeningeal Melanocytosis: A Rare and Challenging Diagnosis. J Neurosci Neurol Disord. 2024; 8: 047-049.
DOI: 10.29328/journal.jnnd.1001096
Copyright License: © 2024 Machado S, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Neoplasia; Melanocytosis; Leptomeninges; Nervous system; Diagnosis
Primary Diffuse Leptomeningeal Melanocytosis: A Rare and Challenging Diagnosis
Stefano Machado1*, Diogo Fernandes dos Santos1, Andrea De Martino Luppi2, Vynícius Vieira Guimarães2 and Ana Cristina Araújo Lemos da Silva3
1Neurology, Clinical Hospital of the Federal University of Uberlandia UFU/EBSERH, Brazil
2Radiology, Clinical Hospital of the Federal University of Uberlandia UFU/EBSERH, Brazil
3Pathology, Clinical Hospital of the Federal University of Uberlandia UFU/EBSERH, Brazil
*Address for Correspondence: Stefano Machado, MD, Neurology, Clinical Hospital of the Federal University of Uberlandia UFU/EBSERH, Brazil, Email: stefanomachadomed@gmail.com
Primary melanocytic neoplasms of the central nervous system are rare entities and can present in different clinical forms with mild and non-specific symptoms (such as headache and tinnitus) to severe and limiting symptoms (focal deficits and intracranial hypertension), mimicking the most diverse pathologies. In addition to the peculiar changes in imaging tests, diagnosis is always a challenge given the multitude of possible differential diagnoses, including aseptic meningitis. Given this, we bring here the case of a 59-year-old patient who attended care due to headache and vertigo followed by involvement of the cranial nerves and spinal cord, corroborated by physical examination and imaging study suggesting diffuse involvement of the meninges, which was subsequently confirmed by anatomopathological examination as a primary melanocytic neoplasm of the central nervous system but ended up dying due to complications resulting from late diagnosis. The objective of this work is to raise awareness about the possibility of this pathology as a differential diagnosis in these cases where there are often frustrating clinical manifestations but with changes in imaging tests, to enable an early diagnosis and consequently the possibility of a better therapeutic result, in addition to a brief review of the propaedeutic findings of this pathology.
Primary diffuse leptomeningeal melanocytosis is a rare disease with benign histopathological characteristics. Leptomeningeal melanocytosis describes primary melanocytic lesions of the central nervous system, which extensively affect the leptomeninges. This disease originates from melanocytes originating from neural crest precursors during the embryonic period [1]. Diagnosis is sometimes delayed due to symptoms, when present, that are non-specific, and the condition is misdiagnosed like other diseases. Despite its non-malignant characteristics, its extent of involvement limits curative surgical treatments, in addition to generating morbidity (intracranial hypertension, focal deficits,...) [2] and secondary clinical complications. Given the rarity, there are still no specific treatment regimens, with current case reports limited to extrapolation of the treatment of malignant pathologies and the service’s experience. In this case report we present a patient with a late diagnosis of diffuse leptomeningeal melanocytosis to illustrate and reinforce the clinical and laboratory findings to enable early suspicion and identification.
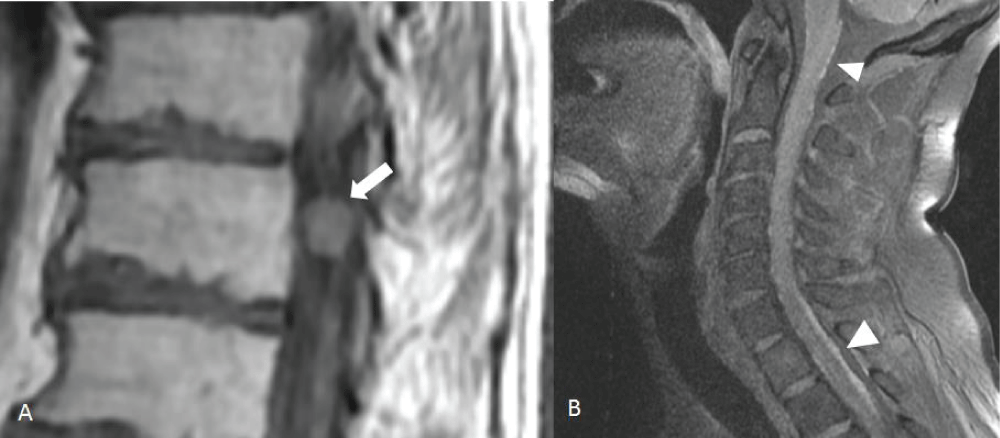
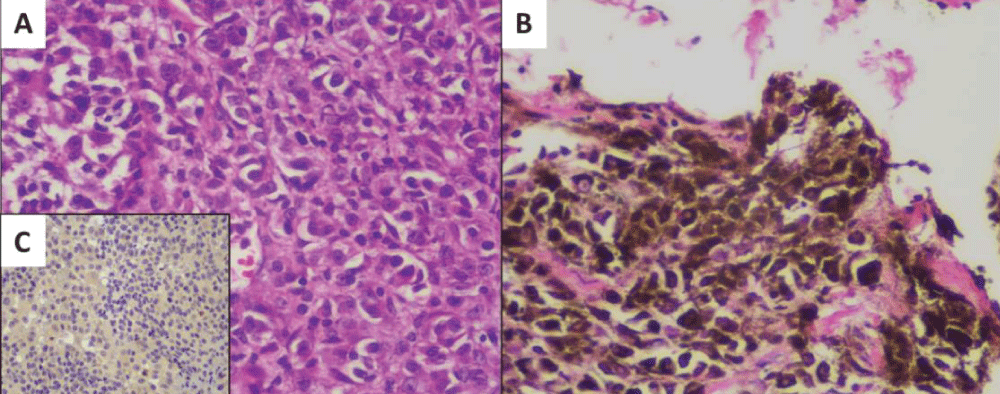
This is a male patient, 59 years old, previously healthy, with no skin lesions, with refractory holocranial headache and vertigo that lasted 8 months, which evolved with decreased visual acuity, paraparesis, and pyramidalism when treated at our service. At the first evaluation, he presented with bilateral papillary edema, multidirectional nystagmus evoked when looking, sensitive level T10/T11, and paraparesis already with signs of pyramidal release. Magnetic resonance imaging investigation showed diffuse enhancement of the leptomeninges, in addition to intradural and extramedullary nodular formation at the level of T11 (Figure 1). The cerebrospinal fluid showed hyperproteinorrachia (167.4 mg/dL) with normal cellularity and CT of the chest and abdomen showed no changes. After extensive investigation, he underwent surgical intervention which revealed blackened leptomeninges (Figure 2), and a biopsy of the lesion was performed which confirmed well-differentiated melanocytic neoplasia (Figure 3). Faced with a generalized condition without definitive curative therapy, he underwent palliative care but died months later due to clinical complications.
Figure 1: MR images of the vertebral spine: (A) T1WI hyperintense lesion at the level of T11 (white arrow), intradural and extramedullary and (B) T1WI fat-sat hyperintensity on the pial surface, close to the posterior aspect of the spinal cord, in the craniocervical and cervicothoracic junctions (white arrowheads), due to the ferromagnetic properties of melanin.
Figure 2: Macroscopic image of leptomeninges during surgery.
Figure 3: Histopathologic Features of Primary Diffuse Leptomeningeal Melanocytosis A and B - (H&E) polygonal cells with round nuclei, prominent eosinophilic nucleolus, moderate cytoplasm, sometimes containing abundant melanin-type brownish pigment, occasionally extracellular (20X); C) Immunostain Ki 67: index of 2.1%, with a maximum of one mitosis in 10 HPF (10x), suggestive of low proliferative potential of the tumor.
Primary melanocytic neoplasia of the central nervous system represents a spectrum of rare tumors that are derived from melanocytes originating in the neural crest (melanocyte precursors, in the embryonic period, migrate via the dorsolateral route to the skin, mucous membranes of the aerodigestive and urogenital tracts, uvea and leptomeninges) [1,2] and is classified as a circumscribed form that includes melanocytoma (benign or low grade) and melanoma (malignant) and diffuse forms that comprise melanocytosis (diffuse proliferation of leptomeningeal melanocytes with a histologically benign appearance) [3] and melanocytosis (aggressive dissemination of histologically atypical or malignant melanocytes) [2].
Leptomeningeal melanocytosis consists of diffuse melanocytic proliferation exhibiting histologically benign features without atypia, mitosis, necrosis, or invasion of the brain parenchyma and may present a positive immunohistochemical reaction to anti-melanoma antibody (HMB-45), S-100 protein, SOX10, and vimentin antibodies, and by a negative reaction to epithelial membrane antigen (EMA) [1,4,5]. The first report of such tumors dates back to 1859 by Virchow. It appears more frequently in children, as an imaging finding, mainly associated with the congenital syndrome of neurocutaneous melanosis, but it can also occur in adults [1].
The estimated annual incidence of primary leptomeningeal melanocytic neoplasms is approximately 1 in 10 million [6]. The symptoms presented can be very varied depending on the site of involvement, such as headache, intracranial hypertension, hydrocephalus, subarachnoid hemorrhage, focal neural deficits, and seizures [2]. The main differential diagnoses are subarachnoid hemorrhage, aseptic meningitis, neurosarcoidosis, tuberculous meningitis, and neoplastic meningitis due to metastatic melanoma [7].
Some of the imaging findings that suggest the diagnosis of melanocytic neoplasia of the central nervous system are the presentation of melanin on magnetic resonance imaging, which can be seen hyperintense on T1 weighting, and hypointense on T2, with intense post-contrast enhancement, low signal on gradient echo T2*-weighted sequence and susceptibility-weighted imaging [3,8,9].
The genetic/molecular field of this pathology is still limited. There are reports, in adults, of activation of mutations in genes that encode G proteins (GNAQ and GNA11) and, in children with neurocutaneous melanosis inactivation of BAP1 and mutations of SF3B1, EIF1AX, and NRAS [7].
Treatment varies depending on the site of involvement, extent, aggressiveness, and molecular profile [2]. As for therapies, surgical intervention becomes limited given the extent of leptomeningeal involvement. Regarding clinical therapies, there is little data in the current literature, with reports of some cases with good temporary responses [2,10].
Primary melanocytic neoplasms of the central nervous system are a rare entity and can have a wide spectrum of initial presentation with non-specific symptoms, such as the case presented, making their suspicion and diagnosis a challenge. Given the scarcity of data, which is limited to just a few case reports, the treatments used as a therapeutic guide are based on personal and/or institutional biases and preferences. There is still a need for more studies on prognosis and targeted treatment, mainly with chemotherapy and radiotherapy.
The authors declare for all due purposes that the work is not financed/sponsored, consent to publication and waive copyright, without conflicts of interest.
Institution carrying out the work: Clinical Hospital of the Federal University of Uberlandia UFU/EBSERH
- Küsters-Vandevelde HV, Küsters B, van Engen-van Grunsven AC, Groenen PJ, Wesseling P, Blokx WA. Primary melanocytic tumors of the central nervous system: a review with focus on molecular aspects. Brain Pathol. 2015 Mar;25(2):209-26. doi: 10.1111/bpa.12241. PMID: 25534128; PMCID: PMC8029366.
- Baumgartner A, Stepien N, Mayr L, Madlener S, Dorfer C, Schmook MT, Traub-Weidinger T, Lötsch-Gojo D, Kirchhofer D, Reisinger D, Hedrich C, Arshad S, Irschik S, Boztug H, Engstler G, Bernkopf M, Rifatbegovic F, Höller C, Slavc I, Berger W, Müllauer L, Haberler C, Azizi AA, Peyrl A, Gojo J. Novel Insights into Diagnosis, Biology and Treatment of Primary Diffuse Leptomeningeal Melanomatosis. J Pers Med. 2021 Apr 12;11(4):292. doi: 10.3390/jpm11040292. PMID: 33921303; PMCID: PMC8069125.
- Hossain FA, Marquez HJ, Veltkamp DL, Xie SQ, Klesse LJ, Timmons CF, Pfeifer CM. CT and MRI findings in leptomeningeal melanocytosis. Radiol Case Rep. 2019 Dec 18;15(3):186-189. doi: 10.1016/j.radcr.2019.11.006. PMID: 31890065; PMCID: PMC6928303.
- Painter TJ, Chaljub G, Sethi R, Singh H, Gelman B. Intracranial and intraspinal meningeal melanocytosis. AJNR Am J Neuroradiol. 2000 Aug;21(7):1349-53. PMID: 10954294; PMCID: PMC8174895.
- Liu ZQ, Liu C, Fu JX, He YQ, Wang Y, Huang TX. Primary intramedullary melanocytoma presenting with lower limbs, defecation, and erectile dysfunction: A case report and review of the literature. World J Clin Cases. 2021 Oct 6;9(28):8616-8626. doi: 10.12998/wjcc.v9.i28.8616. PMID: 34754876; PMCID: PMC8554421.
- Hsieh YY, Yang ST, Li WH, Hu CJ, Wang LS. Primary leptomeningeal melanoma mimicking meningitis: a case report and literature review. J Clin Oncol. 2015 Apr 20;33(12):e57-61. doi: 10.1200/JCO.2013.50.0264. Epub 2014 Mar 17. PMID: 24637995.
- Selvarajan JMP, Epari S, Sahu A, Dasgupta A, Chatterjee A, Gupta T. Pearls & Oy-sters: Primary Diffuse Leptomeningeal Melanocytosis: A Diagnostic Conundrum. Neurology. 2023 Aug 1;101(5):e576-e580. doi: 10.1212/WNL.0000000000207195. Epub 2023 Mar 6. PMID: 36878703; PMCID: PMC10401691.
- Smith AB, Rushing EJ, Smirniotopoulos JG. Pigmented lesions of the central nervous system: radiologic-pathologic correlation. Radiographics. 2009 Sep-Oct;29(5):1503-24. doi: 10.1148/rg.295095109. PMID: 19755608.
- Pirini MG, Mascalchi M, Salvi F, Tassinari CA, Zanella L, Bacchini P, Bertoni F, D'Errico A, Corti B, Grigioni WF. Primary diffuse meningeal melanomatosis: radiologic-pathologic correlation. AJNR Am J Neuroradiol. 2003 Jan;24(1):115-8. PMID: 12533338; PMCID: PMC8148940.
- Palacka P, Slopovsky J, Makovnik M, Kajo K, Obertova J, Mego M. A case report of a patient with inoperable primary diffuse leptomeningeal melanomatosis treated with whole-brain radiotherapy and pembrolizumab. Medicine (Baltimore). 2022 Jan 21;101(3):e28613. doi: 10.1097/MD.0000000000028613. PMID: 35060532; PMCID: PMC8772673.