Case Report
Herpes simplex virus (HSV)-1 encephalitis can induce chronic anti-N-methyl-D-aspartate receptor (NMDAR) encephalitis

Susanne Buechner1*, Gabriele J Sixt2 and Igor Florio3
1Department of Neurology, Regional General Hospital of Bolzano/Bozen, Lorenz Boehler Street 5, 39100 Bolzano/Bozen, Italy2Department of Neurology, Regional General Hospital of Bolzano/Bozen, Bolzano/Bozen, Italy
3Department of Neurology, Regional General Hospital of Bolzano/Bozen, Bolzano/Bozen, Italy
*Address for Correspondence: Susanne Buechner, Department of Neurology, Regional General Hospital of Bolzano/Bozen, Lorenz Boehler Street 5, 39100 Bolzano/Bozen, Italy, Tel: +39-0471-908589; Fax: +39-0471-908591; Email: [email protected]
Dates: Submitted: 12 July 2018; Approved: 26 July 2018; Published: 27 July 2018
How to cite this article: Buechner S, Sixt GJ, Florio I. Herpes simplex virus (HSV)-1 encephalitis can induce chronic anti-N-methyl-D-aspartate receptor (NMDAR) encephalitis. J Neurosci Neurol Disord. 2018; 2: 033-038. DOI: 10.29328/journal.jnnd.1001012
Copyright License: © 2018 Buechner S, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Herpes simplex virus-1 encephalitis; Anti-NMDA receptor encephalitis; Post-viral autoimmune encephalitis; Epileptic seizures; Immunotherapy
Abbreviations: CNS: Central Nervous System; CSF: Cerebrospinal Fluid; CT: Computed Tomography; EEG: Electric Encephalography; GABA: γ-Amino-Butyric Acid; HSV: Herpes Simplex Virus; IgIV: Immunoglobulins; NMDAR: N-Methyl-D-Aspartate Receptor; PCR: Polymerase Chain Reaction; VVI: Ventricle-Ventricle-Inhibited (Kind of Pacemaker Program); WBC: White Blood Cell
Abstract
Herpes simplex virus (HSV)-1 encephalitis is the most common infectious cause of sporadic encephalitis. Despite treatment with acyclovir, HSV encephalitis is still associated with severe morbidity characterized by persistent neurological deficits. HSV encephalitis usually follows a monophasic course, however, some patients might develop relapsing symptoms caused by the formation of auto-antibodies directed against the N-methyl-D-aspartate receptor (NMDAR). Here we present an 82-year-old male patient with HSV encephalitis who developed shortly after his hospital discharge a Post-HSV NMDAR encephalitis, characterized by recurrent epileptic seizures and deterioration of his residual aphasia. First-line immunotherapy with intravenous immunoglobulins (IgIV) was administered and the patient returned almost to his baseline residual deficits of HSV encephalitis. Subsequently, he presented with recurrent relapses of NMDAR encephalitis. Since periodic treatment with IgIV has been started the patient is seizure-free and his neuropsychiatric condition is stable. In conclusion, the recognition of Post-HSV NMDAR encephalitis is very important because neurological manifestations can markedly improve with immunotherapy. Interestingly, in some patients cerebral HSV infection seems to trigger a chronic inflammatory disorder with persistent autoimmune activation which requires chronic treatment.
Introduction
Herpes simplex virus (HSV)-1 encephalitis is the most common infectious cause of sporadic encephalitis with an incidence worldwide estimated to be between 2 and 4 cases/1,000,000 [1]. Despite antiviral treatment with acyclovir, HSV encephalitis remains a devastating condition with significant morbidity and mortality. The disease usually follows a monophasic course but 5%-27% of the patients develop a neurologic relapse within weeks or months after the initial event [1]. In some cases the pathogenesis of the relapse represents a “true” recrudescence of viral encephalitis. In other cases the relapse seems to be immune-mediated rather than a viral reactivation [1]. Since 2013 increasing reports of autoimmune encephalitis associated with anti-N-methyl-D-aspartate receptor (NMDAR) antibodies after HSV encephalitis have been published, which support the likelihood that central nervous system (CNS) HSV infection may trigger an autoimmune response [2]. Post-HSV NMDAR encephalitis has been mainly described in children and young and middle-aged adults [2]. In this case report we present an 82-year-old male patient with HSV encephalitis who developed shortly after his hospital discharge an anti-NMDAR encephalitis, characterized by recurrent epileptic seizures and worsening of his residual aphasia. First-line immunotherapy with intravenous immunoglobulins (IgIV) was successfully administered, however, subsequently, the patient presented with recurrent relapses of NMDAR encephalitis. It seems that cerebral HSV infection had triggered a chronic inflammatory disorder with persistent autoimmune activation, therefore chronic immunotherapy was indicated.
Case Report
During a vacation, an 82-year old man with a VVI pacemaker and medical history positive for atrial fibrillation, under pharmacological treatment with oral anticoagulants and for arterial hypertension, was admitted to the emergency room because of trouble speaking, mental confusion and moderate fever for 5 days. Brain computed tomography (CT) was negative for acute abnormalities, especially for ischemic or hemorrhagic stroke, while laboratory findings demonstrated a severe hyponatremia (113 mmol/l) which was thought to be the reason for the patient’s neurological condition. Back in his home country the patient was admitted to our department of Neurology, due to persistent non-fluent aphasia and recurrent episodes of psychomotor agitation and reduced levels of consciousness. This time the CT scan revealed a mild hypodense lesion in the left temporal region and insular lobe. Electric encephalography (EEG) findings included periodic discharges and focal slowing in the left fronto-temporal areas, sometimes with contralateral diffusion (Figure 1). A cerebrospinal fluid (CSF) analysis showed 81 white blood cells (WBC)/mcl, an increased lactate concentration (2.98 mmol/l) and hyperproteinorachia (105 mg/dl). Empiric treatment with acyclovir (750 mg every 8 hours) and ceftriaxone (2 gr/day) was started. As the detection of HSV-1 polymerase chain reaction (PCR) in CSF was positive, indicating the diagnosis of HSV encephalitis, antibiotic therapy was stopped. A serum and CSF laboratory investigation of auto-antibodies targeting neuronal antigens was negative. During 19 days of antiviral treatment the patient demonstrated a slow but progressive clinical recovery. He was discharged for inpatient cognitive rehabilitation because of a mild residual aphasia. Five days later the patient was readmitted to our department because of recurrent focal seizures, characterized by myoclonic movements of his right-side extremities, which had started the day before and which finally concluded with secondary generalization and worsening of the patient’s residual aphasia. In the acute setting, the brain CT showed the already known lesion in the left temporal-insular region, while the EEG was positive for a predominantly left hemispheric convulsive status epilepticus. The latter was successfully treated with benzodiazepines; a chronic anticonvulsive treatment with levetiracetam was started. A new CSF analysis showed 17 WBC/mcl and hyperproteinorachia (84 mg/dl). At that time, PCR testing was negative for HSV-1, while anti-NMDA receptor antibodies were positive in the CSF (titer 1:64) leading to the diagnosis of Post-HSV NMDAR encephalitis. First-line immunotherapy with intravenous immunoglobulins (IgIV) (0.4 g/kg/day) was given for 5 days, associated to logopedic rehabilitation. The patient demonstrated a substantial improvement of his neuropsychiatric abnormalities and no more seizures, returning almost to his baseline residual deficits of HSV encephalitis. He was dismissed with anti-epileptic medication (levetiracetam 2000 m/day) and resumed his cognitive rehabilitation.
Figure 1: EEG of the patient: Periodic discharges and focal slowing in the left fronto-temporal areas, visible in an early stage of the HSV-1 encephalitis.
After two and a half months of well-being the patient developed again recurrent focal epileptic seizures; furthermore, his residual mild aphasia deteriorated significantly. Brain CT scan confirmed the already known lesion in the left temporal-insular region. Immunotherapy with IgIV was successfully repeated and the patient was dismissed with the diagnosis of relapsing Post-HSV NMDAR encephalitis. Three weeks later the patient demonstrated a re-worsening of his aphasic deficits, but he also developed mental confusion, apraxia and a mild right arm motor weakness. Initially, a new relapse of the autoimmune-encephalitis was hypothesized, therefore treatment with IgIV was started again, supplemented at that time with high doses of steroids. Brain CT was repeated, which unexpectedly revealed an acute/sub-acute left hemispheric subdural hematoma (19 mm) provoking mild midline shifting. The patient’s history was apparently mute for recent head injuries, but he was still on oral anticoagulant therapy with warfarin because of his atrial fibrillation. The patient underwent successfully neurosurgery, and postoperative course was uneventful. However, the patient did not return to his previous neuropsychiatric state. At discharge he presented with moderate, mainly expressive, aphasia and a mild right arm paresis; oral steroid treatment (prednisone 50 mg) was continued. One and a half months later the patient’s aphasia deteriorated again, probably due to non-convulsive epileptic seizures. Brain CT results were negative for acute abnormalities, while a repeated CSF analysis demonstrated a still positive, even though lower, anti-NMDA receptor antibody titer (1:1). Five days of treatment with IgIV and an increase of levetiracetam dosage (3000 mg/day) were prescribed.
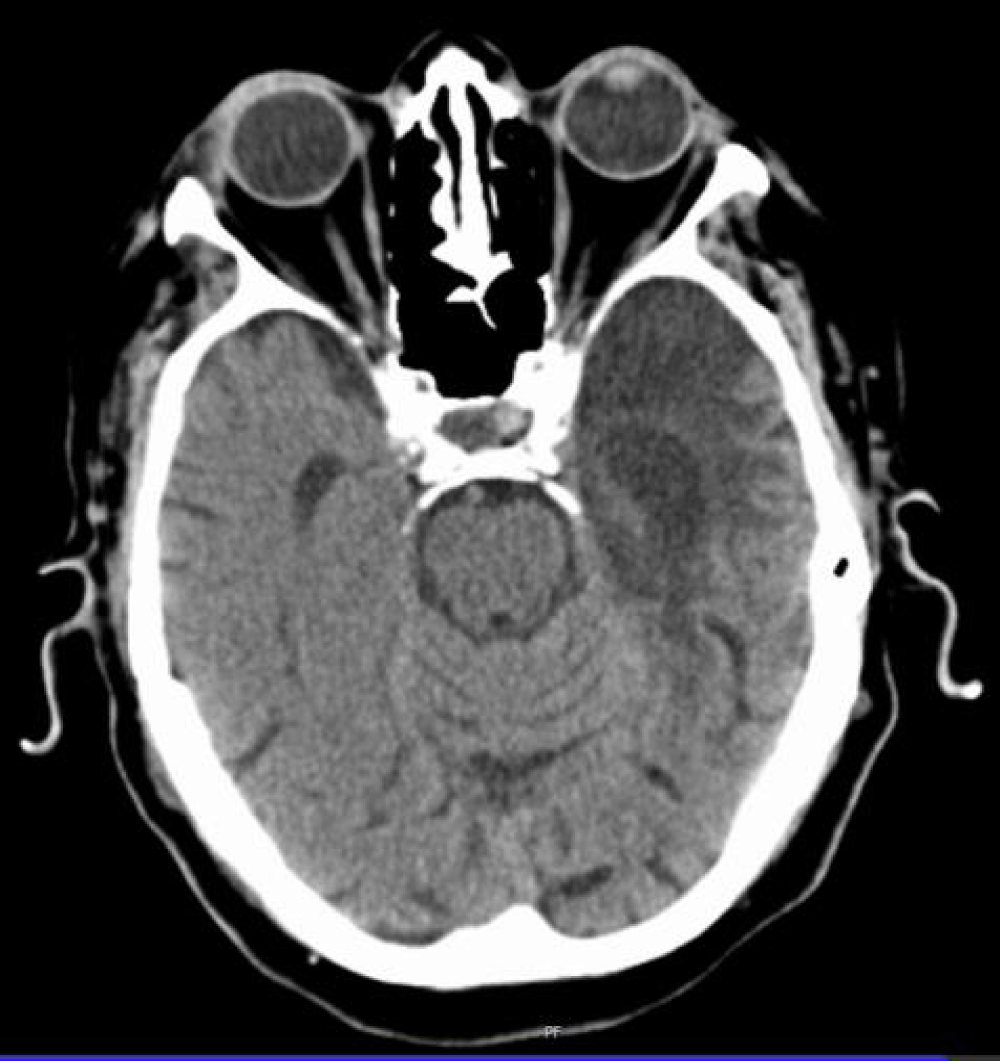
After several NMDAR-encephalitis’ reacutizations, second-line treatment with rituximab was finally considered. As the patient was twice in the “grey zone” with QuantiFERON-tuberculosis testing, our colleagues of the Infectious Diseases Department recommended a long-lasting chemoprophylaxis in order to avoid a possible tuberculosis activation under rituximab treatment. This latter therapeutic proposal was not accepted by the patient’s family, therefore periodic treatment with IgIV was started (35 g/day, for 2 days, every 4-6 weeks), while the apparently unsuccessful steroid oral medication was suspended. Furthermore, lacosamide add-on therapy for epilepsy was introduced and thanks to blood regression on brain CT, the patient started oral anticoagulation with dabigatran. After more than one and a half years, the now 84-year-old patient hasn’t had any more epileptic seizures and his neuropsychiatric condition, characterized mainly by an expressive aphasia, is still stable. Figure 2 shows the patient’s last brain CT control (Figure 2).
Figure 2: Brain CT of the patient: Voluminous porencephalic area in left temporal-insular region caused by the previous HSV-1 encephalitis.
Discussion
Patients with HSV encephalitis should be monitored closely after their discharge as they might develop a Post-HSV NMDAR encephalitis. Relapses of neurological symptoms after HSV encephalitis have been reported in 5% to 27% of the patients, with a higher frequency in children, in whom the latency between HSV- and anti-NMDAR encephalitis is also significantly shorter than in adults [2]. The recognition of post-viral autoimmune encephalopathy might be difficult in adults as they tend to present with psychiatric and cognitive symptoms that may be difficult to distinguish from the residual deficits of HSV encephalitis [3]. In addition, the symptom presentation may occur in contiguity with HSV encephalitis, suggesting a persisting viral infection [3]. In children however, the clinical presentation of the relapse, i.e. of the autoimmune encephalitis, is relatively stereotyped, consisting mainly of the appearance of choreoathetosis and reduced levels of consciousness [3]. The less recognizable relapse in adults might be one reason why NMDAR encephalitis after HSV encephalitis has been less frequently reported in elderly patients. In our 82-year-old patient the clinical worsening after HSV encephalitis, characterized by recurrent epileptic seizures, made it quite easy to suppose a post-viral autoimmune encephalitis, as a completely new neurological symptom had appeared. On the other hand, prompt recognition of HSV-induced anti-NMADR encephalitis is important because immunotherapy may provide substantial clinical improvement [1-3]. Treatment consists in first- and second-line immunotherapy, including corticosteroids, plasma-exchanges, IgIV, rituximab, and other immunosuppressive strategies [1-3]. Immunotherapy given for immune-mediated postinfectious HSV encephalopathy seems to be safe and does not predispose patients to viral reactivation, therefore additional long-term antiviral therapy is not necessary [2]. In our patient, first-line immunotherapy consisted of IgIV which had been demonstrated to be effective and well-tolerated right from the beginning. As our patient relapsed on average every 4-6 weeks, periodic IgIV treatment was started more than one and a half years ago. Corticosteroids were not given to the patient initially because of his poorly controlled arterial hypertension and recurrent episodes of psychomotor agitation. Finally, prednisone had been added to treatment, however, only for some months because it seemed to be ineffective. Second-line treatment was ruled out because of a “grey zone” tuberculosis test result with indication for long-lasting chemoprophylaxis which was not accepted by the patient’s family.
So far, the patient has been seizure free under the current immunotherapy, and his neuropsychiatric condition is still stable. It is true, that lacosamide was added to the patient’s therapy, and therefore it is not clear if his epilepsy is now successfully controlled by the anticonvulsant polytherapy (levetiracetam+ lacosamide) and/or the periodic IgIV infusions. However, seizures appear frequently after HSV encephalitis, but might be mainly a consequence of the post-encephalitic autoimmune process and not secondary to cortical scarring [4]. The mechanism of epileptogenesis is not easily explained. NMDAR-antibodies react with the NMDA receptors, causing their internalization into the cells which provokes a reversible NMDAR hypofunction. On the other hand, several NMDAR blockers inducing NMDAR hypofunction, exert an antiepileptic effect [5-6]. However, it seems, that an antibody-mediated decrease of NMDAR inactivates GABAergic neurons, which leads to disinhibition of excitatory pathways and increase of glutamate in the extracellular space of the brain, which finally provokes the epileptic seizures [5-6]. The exact pathogenesis of the Post-HSV NMDAR encephalitis is not known yet, however several pathogenic mechanisms have been considered such as molecular mimicry or antigen spreading [2]. For sure, HSV-1 causes an aggressive necrotizing infection of neurons and glial cells, and a vigorous intrathecal inflammatory response in limbic structures with persistent immune activation [4]. Due to this significant inflammatory and immunologic reaction triggered by HSV, immunotherapy could play an important role also in the management of the acute phase of HSV encephalitis. In the literature, several cases have been described where patients had received simultaneous administration of acyclovir and steroids in the acute encephalitic phase, however, many of them nevertheless developed an autoimmune encephalopathy [7]. The non-beneficial effect of adjunctive steroids in those patients confirms that the role of the anti-NMDAR antibodies in HSV encephalitis is still nebulous [8]. Frequently, anti-NMDAR antibodies and other kinds of auto-antibodies are detected in patients with HSV encephalitis. However, the clinical course of viral encephalitis is often identical in patients with or without auto-antibodies and only some patients finally develop an autoimmune encephalopathy [8]. Maybe the production of auto-antibodies represents a nonspecific immune activation, therefore further factors such as the patient’s immunocompetence and/or the brain lesion volume caused by HSV encephalitis might be involved in the development of the autoimmune encephalitis.
Interestingly, it seems that the intrathecal autoimmunization secondary to the HSV-triggered CNS inflammation might be, at least in some cases, a continuous process which contributes to persisting neurocognitive symptoms after HSV encephalitis [4]. HSV-1 establishes a lifelong infection which might be a trigger for a chronic autoimmune activation [1]. Some authors have reported a case series supporting the hypothesis of a chronic inflammatory disorder secondary to a persistent post-infectious autoimmunity with long-term disease progression, which might even lead to hippocampal sclerosis [9]. Other authors have supposed that the persistence of some CSF cytokines/chemokines after HSV encephalitis might lead to a long-lasting antibody production, provoking a refractory anti-NMDAR encephalitis [10]. In summary, postviral anti-NMDAR encephalitis might become a chronic disease in contrast to “classic” anti-NMDAR encephalitis, which demonstrates mostly a monophasic course (relapses in only around 12% within the first 2 years) [5]. In order to prevent a chronic NMDAR encephalitis, second-line immunotherapy should be promptly considered, also in an early stage of autoimmune encephalopathy [10]. In some patients long-lasting immunotherapy might be indicated. A correct management might bring the patients back to their residual deficits of HSV encephalitis, avoiding further disease progression. Taken together, observations suggest that a chronic post-viral autoimmune state could be an explanation of why our patient suffers from “relapsing” Post-HSV NMDAR encephalitis, characterized by recurrent epileptic seizures and/or aphasia worsening, and why the periodic IgIV treatment seems to be helpful.
Conclusion
In conclusion, post-viral autoimmune encephalitis should be considered also in elderly patients with previous HSV encephalitis, especially in those with prolonged symptoms or re-worsening deficits. The less recognizable symptoms of HSV-induced anti-NMADR encephalitis in adults may provoke a delay in diagnosis, however, its recognition is important because immunotherapy may provide substantial clinical improvement avoiding further disease progression. For that reason, a very close and long-lasting monitoring of patients with previous HSV encephalitis is required, also because CNS HSV infection seems to trigger, at least in some patients, a chronic inflammatory disorder with persistent autoimmune activation. It seems that post-viral anti-NMDAR encephalitis might become a chronic disease in contrast to the “classic” anti-NMDAR encephalitis, which is mostly monophasic.
Acknowledgement
We are grateful to the Patient and his relatives who agreed to use data for publication, and thankful to all colleagues and friends who performed proofreading.
Consent
Signed informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consents is available for review by the Editor of this journal.
References
- Bradshaw MJ, Venkatesan A. Herpes Simplex Virus-1 Encephalitis in Adults: Pathophysiology, Diagnosis, and Management. Neurotherapeutics. 2016; 13: 493-508. Ref.: https://tinyurl.com/y896nyme
- Nosadini M, Mohammad SS, Corazza F, Ruga EM, Kavitha Kothur, et al. Herpes simplex virus-induced anti-N-methyl-D-aspartate receptor encephalitis: a systemic literature review with analysis of 43 cases. Developmental Medicine & Child Neurology. 2017; 59: 796-805. Ref.: https://tinyurl.com/y9qoyq2r
- Armangue T, Moris G, Cantarin-Extremera V, Conde CE, Rostasy K, et at. Autoimmune post-herpes simplex encephalitis of adults and teenagers. Neurology. 2015; 85: 1736-1743. Ref.: https://tinyurl.com/y9r6hdfs
- Westman G, Studahl M, Ahlm C, Eriksson BM, Persson B, et al. N-methyl-D-aspartate receptor autoimmunity affects cognitive performance in herpes simplex encephalitis. Clin Microbiol Infect. 2016; 22: 934-940. Ref.: https://tinyurl.com/yd8m4na3
- Kovac S, Alferink J, Ahmetspahic D, Arolt V, Melzer N. Update Anti-N-Methyl-D-Aspartat-Rezeptor-Enzephalitis. Nervenarzt. 2018; 89: 99-112. Ref.: https://tinyurl.com/y9np7ye4
- Bien CG, Bauer J. Autoimmune Epilepsies. Neurotherapeutics. 2014; 11: 311-318. Ref.: https://tinyurl.com/y7hgfc2e
- Schein F, Gagneux-Brunon A, Antoine JC, Lavernhe S, Pillet S, et al. Anti-N-methyl-D-aspartate receptor encephalitis after Herpes simplex virus-associated encephalitis: an emerging disease with diagnosis and therapeutic challenges. Infection. 2017; 45: 545-549. Ref.: https://tinyurl.com/ycjcvyrd
- Linnoila JJ, Binnicker MJ, Majed M, Klein CJ, McKeon A. CSF herpes virus and autoantibody profiles in the evaluation of encephalitis. Neurol Neuroimmunol Neuroinflamm. 2016; 3: e245. Ref.: https://tinyurl.com/y8l4mlsb
- Popkirov S, Ismail FS, Grönheit W, Kapauer M, Wellmer J, et al. Progressive hippocampal sclerosis after viral encephalitis: Potential role of NMDA receptor antibodies. Seizure. 2017; 51: 6-8. Ref.: https://tinyurl.com/y83qkcmo
- Omae T, Saito Y, Tsuchie H, Ohno K, Maegaki Y, et al. Cytokine/chemokine elevation during the transition phase from HSV encephalitis to autoimmune anti-NMDA receptor encephalitis. Brain Dev. 2018; 40: 361-365. Ref.: https://tinyurl.com/yaqahfqb