Abstract
Research Article
A Comparative Study of Metoprolol and Amlodipine on Mortality, Disability and Complication in Acute Stroke
Jayantee Kalita*, Dhiraj Kumar, Nagendra B Gutti, Sandeep K Gupta, Anadi Mishra and Vivek Singh
Published: 04 April, 2025 | Volume 9 - Issue 1 | Pages: 039-045
Stress in acute stroke may increase mortality and complications, but there is a paucity of information on the efficacy of beta blockers over other anti-hypertensive. To report efficacy of metoprolol over amlodipine in reducing mortality, disability and infections in acute stroke. CT/MRI confirmed stroke patients within 3 days of onset were included whose age was 18 to 75 years. Patients with secondary intracerebral hemorrhage, organ failure, pregnancy, malignancy, and immunosuppressant or on beta-blocker/amlodipine were excluded. Stroke risk factors, Glasgow Coma Scale (GCS) score, National Institute of Health Stroke Scale (NIHSS) score and CT/MRI findings were noted. Patients with a blood pressure of > 160/90 mm of Hg were randomized using 1:1 randomization to metoprolol (25 mg on day 1, 50 mg if BP is not controlled) or amlodipine (2.5 mg on day 1, then 5 mg then 10 mg on, subsequent days if BP is not controlled). Other standard treatment was continued. The primary outcome was mortality at 1 month; secondary outcomes included were in-hospital gastrointestinal hemorrhage, pneumonia, sepsis and 3 months functional outcome based on modified Rankin Scale (mRS). Side effects were noted. 18 (14.4%) patients died; 6 (9.7%) in metoprolol and 12 (19%) in amlodipine (p = 0.20) group. At 3-months, 66 patients had good outcome; 45 (80.4%) in metoprolol and 21 (43.3%) in amlodipine group (p < 0.001). The other secondary outcomes were comparable between the two groups. Metoprolol was withdrawn in 6 patients due to bradycardia, and amlodipine in 5 due to hypotension and in 1 due to allergic reaction. Metoprolol is associated with improved functional outcomes in acute stroke compared to amlodipine.
Read Full Article HTML DOI: 10.29328/journal.jnnd.1001108 Cite this Article Read Full Article PDF
Keywords:
Intracerebral hemorrhage; Infarction; Beta-blocker; Calcium channel blocker; Outcome
References
- GBD 2019 Stroke Collaborators. Global, regional, and national burden of stroke and its risk factors, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet Neurol. 2021;20(10):795-820. Available from: https://doi.org/10.1016/s1474-4422(21)00252-0
- Kalita J, Goyal G, Kumar P, Misra UK. Intracerebral hemorrhage in young patients from a tertiary neurology center in North India. J Neurol Sci. 2014;336(1-2):42-7. Available from: https://doi.org/10.1016/j.jns.2013.09.037
- Hankey GJ. Population Impact of Potentially Modifiable Risk Factors for Stroke. 2020;51(3):719-728. Available from: https://doi.org/10.1161/strokeaha.119.024154
- Lackland DT, Roccella EJ, Deutsch AF, Fornage M, George MG, Howard G, et al. American Heart Association Stroke Council; Council on Cardiovascular and Stroke Nursing; Council on Quality of Care and Outcomes Research; Council on Functional Genomics and Translational Biology. Factors influencing the decline in stroke mortality: a statement from the American Heart Association/American Stroke Association. 2014;45(1):315-53. Available from: https://doi.org/10.1161/01.str.0000437068.30550.cf
- Algin A, Inan I. The role of radiologic, clinical and biochemical parameters in prediction of stroke mortality. Neurosciences (Riyadh). 2019;24(2):110-114. Available from: https://doi.org/10.17712/nsj.2019.2.20180021
- Chen Z, Venkat P, Seyfried D, Chopp M, Yan T, Chen J. Brain-Heart Interaction: Cardiac Complications After Stroke. Circ Res. 2017;121(4):451-468. Available from: https://doi.org/10.1161/circresaha.117.311170
- Maier IL, Karch A, Mikolajczyk R, Bähr M, Liman J. Effect of beta-blocker therapy on the risk of infections and death after acute stroke--a historical cohort study. PLoS One. 2015;10(2):e0116836. Available from: https://doi.org/10.1371/journal.pone.0116836
- Dorrance AM, Fink G. Effects of Stroke on the Autonomic Nervous System. Compr Physiol. 2015;5(3):1241-63. Available from: https://doi.org/10.1002/cphy.c140016
- Zhu H, Wang Z, Yu J, Yang X, He F, Liu Z, et al. Role and mechanisms of cytokines in the secondary brain injury after intracerebral hemorrhage. Prog Neurobiol. 2019;178:101610. Available from: https://doi.org/10.1016/j.pneurobio.2019.03.003
- Maida CD, Norrito RL, Daidone M, Tuttolomondo A, Pinto A. Neuroinflammatory Mechanisms in Ischemic Stroke: Focus on Cardioembolic Stroke, Background, and Therapeutic Approaches. Int J Mol Sci. 2020;21(18):6454. Available from: https://doi.org/10.3390/ijms21186454
- Prass K, Meisel C, Höflich C, Braun J, Halle E, Wolf T, et al. Stroke-induced immunodeficiency promotes spontaneous bacterial infections and is mediated by sympathetic activation reversal by poststroke T helper cell type 1-like immunostimulation. J Exp Med. 2003;198(5):725-36. Available from: https://doi.org/10.1084/jem.20021098
- Koton S, Tanne D, Green MS, Bornstein NM. Mortality and predictors of death 1 month and 3 years after first-ever ischemic stroke: data from the first national acute stroke Israeli survey (NASIS 2004). 2010;34(2):90-6. Available from: https://doi.org/10.1159/000264826
- Barer DH, Cruickshank JM, Ebrahim SB, Mitchell JR. Low dose beta blockade in acute stroke ("BEST" trial): an evaluation. Br Med J (Clin Res Ed). 1988;296(6624):737-41. Available from: https://doi.org/10.1136/bmj.296.6624.737
- Dziedzic T, Slowik A, Pera J, Szczudlik A. Beta-blockers reduce the risk of early death in ischemic stroke. J Neurol Sci. 2007;252(1):53-6. Available from: https://doi.org/10.1016/j.jns.2006.10.007
- Sykora M, Siarnik P, Diedler J; VISTA Acute Collaborators. β-Blockers, Pneumonia, and Outcome After Ischemic Stroke: Evidence From Virtual International Stroke Trials Archive. 2015;46(5):1269-74. Available from: https://doi.org/10.1161/strokeaha.114.008260
- Balla HZ, Cao Y, Ström JO. Effect of Beta-Blockers on Stroke Outcome: A Meta-Analysis. Clin Epidemiol. 2021 Mar 16;13:225-236. Available from: https://doi.org/10.2147/clep.s268105
- Rangel-Frausto MS, Pittet D, Costigan M, Hwang T, Davis CS, Wenzel RP. The natural history of the systemic inflammatory response syndrome (SIRS). A prospective study. 1995;273(2):117-23. Available from: https://pubmed.ncbi.nlm.nih.gov/7799491/
- Misra UK, Kalita J, Srivastava M, Mandal SK. A study of prognostic predictors of supratentorial haematomas. J Neurol. 1996;243(1):96-100. Available from: https://doi.org/10.1007/bf00878539
- de Margerie-Mellon C, Turc G, Tisserand M, Naggara O, Calvet D, Legrand L, et al. Can DWI-ASPECTS substitute for lesion volume in acute stroke? 2013 Dec;44(12):3565-7. Available from: https://doi.org/10.1161/strokeaha.113.003047
- Mandell, Lionel A, and Michael S. Niederman. "Pneumonia." Harrison's Principles of Internal Medicine, 21e. McGraw-Hill Education, 2022. Available from: https://ugc.production.linktr.ee/d40733b1-ae5f-4b54-a04a-59f8dda7e3a8_1-Reduced-Harrison-21st.pdf
- Brant EB, Seymour CW, Angus DC. Sepsis and Septic Shock. In: Loscalzo J, Fauci A, Kasper D, Hauser S, Longo D, Jameson J, editors. Harrison's Principles of Internal Medicine, 21e. McGraw-Hill Education; 2022. Accessed March 06, 2025.
- Singer M, Deutschman CS, Seymour CW, Shankar-Hari M, Annane D, Bauer M, et al. The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). 2016;315(8):801-10. Available from: https://doi.org/10.1001/jama.2016.0287
- Kalita J, Bastia J, Bhoi SK, Misra UK. Systemic Inflammatory Response Syndrome Predicts Severity of Stroke and Outcome. J Stroke Cerebrovasc Dis. 2015;24(7):1640-8. Available from: https://doi.org/10.1016/j.jstrokecerebrovasdis.2015.03.057
- Kalita J, Misra UK, Kumar B. Is β-blocker (atenolol) a preferred antihypertensive in acute intracerebral hemorrhage? Neurol Sci. 2013;34(7):1099-104. Available from: https://doi.org/10.1007/s10072-012-1210-y
- Potter J, Mistri A, Brodie F, Chernova J, Wilson E, Jagger C, et al. Controlling hypertension and hypotension immediately post stroke (CHHIPS)--a randomised controlled trial. Health Technol Assess. 2009;13(9):iii, ix-xi, 1-73. Available from: https://doi.org/10.3310/hta13090
- Savitz SI, Erhardt JA, Anthony JV, Gupta G, Li X, Barone FC, et al. The novel beta-blocker, carvedilol, provides neuroprotection in transient focal stroke. J Cereb Blood Flow Metab. 2000;20(8):1197-204. Available from: https://doi.org/10.1097/00004647-200008000-00005
- Tziomalos K, Giampatzis V, Bouziana SD, Spanou M, Papadopoulou M, Kazantzidou P, et al. Effects of different classes of antihypertensive agents on the outcome of acute ischemic stroke. J Clin Hypertens (Greenwich). 2015;17(4):275-80. Available from: https://doi.org/10.1111/jch.12498
- Sundbøll J, Schmidt M, Horváth-Puhó E, Christiansen CF, Pedersen L, Bøtker HE, et al. Impact of preadmission treatment with calcium channel blockers or beta blockers on short-term mortality after stroke: a nationwide cohort study. BMC Neurol. 2015;15:24. Available from: https://doi.org/10.1186/s12883-015-0279-3
- Eizenberg Y, Grossman E, Tanne D, Koton S. Pre-admission treatment with Beta-blockers in hypertensive patients with acute stroke and 3-month outcome-Data from a national stroke registry. J Clin Hypertens (Greenwich). 2018;20(3):568-72. Available from: https://doi.org/10.1111/jch.13211
- Yang L, Wenping X, Jinfeng Z, Jiangxia P, Jingbo W, Baojun W. Are beta blockers effective in preventing stroke-associated infections? - a systematic review and meta-analysis. Aging (Albany NY). 2022;14(10):4459-70. Available from: https://doi.org/10.18632/aging.204086
- Starr JB, Tirschwell DL, Becker KJ. Increased infections with β-blocker use in ischemic stroke, a β2-receptor mediated process? Neurol Sci. 2017;38(6):967-74. Available from: https://doi.org/10.1007/s10072-017-2877-x
- Westendorp WF, Vermeij JD, Brouwer MC, Roos YB, Nederkoorn PJ, van de Beek D; PASS Investigators. Pre-Stroke Use of Beta-Blockers Does Not Lower Post-Stroke Infection Rate: An Exploratory Analysis of the Preventive Antibiotics in Stroke Study. Cerebrovasc Dis. 2016;42(5-6):506-11. Available from: https://doi.org/10.1159/000450926
- Maier IL, Becker JC, Leyhe JR, Schnieder M, Behme D, Psychogios MN, et al. Influence of beta-blocker therapy on the risk of infections and death in patients at high risk for stroke induced immunodepression. PLoS One. 2018;13(4):e0196174. Available from: https://doi.org/10.1371/journal.pone.0196174
- Freemantle N, Cleland J, Young P, Mason J, Harrison J. Beta Blockade after myocardial infarction: systematic review and meta regression analysis. BMJ. 1999;318(7200):1730-7. Available from: https://doi.org/10.1136/bmj.318.7200.1730
- Heidenreich PA, Lee TT, Massie BM. Effect of beta-blockade on mortality in patients with heart failure: a meta-analysis of randomized clinical trials. J Am Coll Cardiol. 1997;30(1):27-34. Available from: https://doi.org/10.1016/s0735-1097(97)00104-6
- Morelli A, Ertmer C, Westphal M, Rehberg S, Kampmeier T, Ligges S, et al. Effect of heart rate control with esmolol on hemodynamic and clinical outcomes in patients with septic shock: a randomized clinical trial. JAMA. 2013;310(16):1683-91. Available from: https://doi.org/10.1001/jama.2013.278477
- van der Jagt M, Miranda DR. Beta-blockers in intensive care medicine: potential benefit in acute brain injury and acute respiratory distress syndrome. Recent Pat Cardiovasc Drug Discov. 2012;7(2):141-51. Available from: https://doi.org/10.2174/157489012801227274
- Weir CJ, Bradford AP, Lees KR. The prognostic value of the components of the Glasgow Coma Scale following acute stroke. QJM. 2003;96(1):67-74. Available from: https://doi.org/10.1093/qjmed/hcg008
- Das S, Chandra Ghosh K, Malhotra M, Yadav U, Sankar Kundu S, Kumar Gangopadhyay P. Short-term mortality predictors in acute stroke. Ann Neurosci. 2012;19(2):61-7. Available from: https://doi.org/10.5214/ans.0972.7531.12190203
- Saunders DE, Clifton AG, Brown MM. Measurement of infarct size using MRI predicts prognosis in middle cerebral artery infarction. Stroke. 1995;26(12):2272-6. Available from: https://doi.org/10.1161/01.str.26.12.2272
- Mahdy ME, Ghonimi NA, Elserafy TS, Mahmoud W. The NIHSS score can predict the outcome of patients with primary intracerebral hemorrhage. Egypt J Neurol Psychiatry Neurosurg. 2019;55:21. Available from: https://ejnpn.springeropen.com/articles/10.1186/s41983-019-0056-0
- McKeown ME, Prasad A, Kobsa J, Top I, Snider SB, Kidwell C, et al. Midline shift greater than 3 mm independently predicts outcome after ischemic stroke. Neurocrit Care. 2022;36(1):46-51. Available from: https://doi.org/10.1007/s12028-021-01341-x
- Yuan MZ, Li F, Fang Q, Wang W, Peng JJ, Qin DY, et al. Research on the cause of death for severe stroke patients. J Clin Nurs. 2018;27(1-2):450-60. Available from: https://doi.org/10.1111/jocn.13954
- Chen YC, Chen CM, Liu JL, Chen ST, Cheng ML, Chiu DT. Oxidative markers in spontaneous intracerebral hemorrhage: leukocyte 8-hydroxy-2'-deoxyguanosine as an independent predictor of the 30-day outcome. J Neurosurg. 2011;115(6):1184-90. Available from: https://doi.org/10.3171/2011.7.jns11718
- Feibel JH, Hardy PM, Campbell RG, Goldstein MN, Joynt RJ. Prognostic value of the stress response following stroke. JAMA. 1977;238(13):1374-6. Available from: https://pubmed.ncbi.nlm.nih.gov/578192/
- Mehta R, Chinthapalli K. Glasgow coma scale explained. BMJ. 2019;365:l1296. Available from: https://doi.org/10.1136/bmj.l1296
- McNett M. A review of the predictive ability of Glasgow Coma Scale scores in head-injured patients. J Neurosci Nurs. 2007;39(2):68-75. Available from: https://doi.org/10.1097/01376517-200704000-00002
- Hanel RA, Xavier AR, Mohammad Y, Kirmani JF, Yahia AM, Qureshi AI. Outcome following intracerebral hemorrhage and subarachnoid hemorrhage. Neurol Res. 2002;24 Suppl 1:S58-62. Available from: https://doi.org/10.1179/016164102101200041
- Kalita J, Mani VE, Bhoi SK, Misra UK. Spectrum and outcome of acute infectious encephalitis/encephalopathy in an intensive care unit from India. QJM. 2017;110(3):141-8. Available from: https://doi.org/10.1093/qjmed/hcw132
- Kalita J, Singh RK, Misra UK, Kumar S. Evaluation of cerebral arterial and venous system in tuberculous meningitis. J Neuroradiol. 2018;45(2):130-5. Available from: https://doi.org/10.1016/j.neurad.2017.09.005
- Boehme AK, Hays AN, Kicielinski KP, Arora K, Kapoor N, Lyerly MJ, et al. Systemic inflammatory response syndrome and outcomes in intracerebral hemorrhage. Neurocrit Care. 2016;25(1):133-40. Available from: https://doi.org/10.1007/s12028-016-0255-9
Figures:
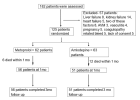
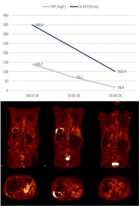
Figure 1
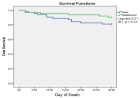
Figure 2

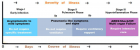
Figure 3
Similar Articles
-
Analysis of early Versus Delayed Carotid Surgery after Acute Ischemic StrokePEROU Sébastien*,DETANTE Olivier,SPEAR Rafaelle,PIRVU Augustin,ELIE Amandine,MAGNE Jean-Luc. Analysis of early Versus Delayed Carotid Surgery after Acute Ischemic Stroke. . 2017 doi: 10.29328/journal.jnnd.1001001; 1: 001-011
-
Long-term clinical outcome of minimally invasive versus open single-level transforaminal lumbar interbody fusion for degenerative lumbar diseases with a minimum follow-up of 2 years: A meta-analysis protocolJohan L Heemskerk*,Oluwaseun Oluwadara Akinduro,William Clifton,Alfredo Quinones-Hinojosa,Kingsley O Abode-Iyamah. Long-term clinical outcome of minimally invasive versus open single-level transforaminal lumbar interbody fusion for degenerative lumbar diseases with a minimum follow-up of 2 years: A meta-analysis protocol. . 2019 doi: 10.29328/journal.jnnd.1001021; 3: 091-095
-
Immunohistochemical expression of Nestin as Cancer Stem Cell Marker in gliomasRasha Mokhtar Abdelkareem*,Afaf T Elnashar,Khaled Nasser Fadle,Eman MS Muhammad. Immunohistochemical expression of Nestin as Cancer Stem Cell Marker in gliomas. . 2019 doi: 10.29328/journal.jnnd.1001027; 3: 162-166
-
Atlantoaxial subluxation in the pediatric patient: Case series and literature reviewCatherine A Mazzola*,Catherine Christie,Isabel A Snee,Hamail Iqbal. Atlantoaxial subluxation in the pediatric patient: Case series and literature review. . 2020 doi: 10.29328/journal.jnnd.1001037; 4: 069-074
-
Impact of mandibular advancement device in quantitative electroencephalogram and sleep quality in mild to severe obstructive sleep apneaCuspineda-Bravo ER*,García- Menéndez M,Castro-Batista F,Barquín-García SM,Cadelo-Casado D,Rodríguez AJ,Sharkey KM. Impact of mandibular advancement device in quantitative electroencephalogram and sleep quality in mild to severe obstructive sleep apnea. . 2020 doi: 10.29328/journal.jnnd.1001041; 4: 088-098
-
Cerebral arterial air embolism with anterior spinal cord syndrome after CT-guided hook-wire localization of Lung mass and pulmonary noduleNoor Sameh Darwich*,Umran Ugur,Mark P Anstadt,J Pedoto. Cerebral arterial air embolism with anterior spinal cord syndrome after CT-guided hook-wire localization of Lung mass and pulmonary nodule. . 2021 doi: 10.29328/journal.jnnd.1001044; 5: 006-015
-
Cortical spreading depolarizations in the context of subarachnoid hemorrhage and the role of ketamineLeandro Custódio do Amaral*. Cortical spreading depolarizations in the context of subarachnoid hemorrhage and the role of ketamine. . 2021 doi: 10.29328/journal.jnnd.1001045; 5: 016-021
-
Endovascular management of tandem occlusions in stroke: Treatment strategies in a real-world scenarioJuan J Cirio*,Celina Ciardi,Matias Lopez,Esteban V Scrivano,Javier Lundquist,Ivan Lylyk,Nicolas Perez,Pedro Lylyk. Endovascular management of tandem occlusions in stroke: Treatment strategies in a real-world scenario. . 2021 doi: 10.29328/journal.jnnd.1001051; 5: 055-060
-
Role of perioperative plasma D-dimer in intracerebral hemorrhage after brain tumor surgery: A prospective studyEstela Val Jordán*,Agustín Nebra Puertas,Juan Casado Pellejero,Concepción Revilla López,Nuria Fernández Monsteirín,Lluis Servia Goixart,Manuel Quintana Díaz,Beatriz Virgos Señor,Silvia Rodríguez Ruiz,Nuria Ramón Coll,Gabriel Jiménez Jiménez,David Fuentes Esteban,Jesús Caballero López. Role of perioperative plasma D-dimer in intracerebral hemorrhage after brain tumor surgery: A prospective study. . 2022 doi: 10.29328/journal.jnnd.1001064; 6: 024-031
-
Circadian temperature rhythms of the healthy and damaged brainShevelev OA*,Petrova MV,Yuriev MY,Mengistu EM. Circadian temperature rhythms of the healthy and damaged brain. . 2022 doi: 10.29328/journal.jnnd.1001065; 6: 032-033
Recently Viewed
-
Cystoid Macular Oedema Secondary to Bimatoprost in a Patient with Primary Open Angle GlaucomaKonstantinos Kyratzoglou*,Katie Morton. Cystoid Macular Oedema Secondary to Bimatoprost in a Patient with Primary Open Angle Glaucoma. Int J Clin Exp Ophthalmol. 2025: doi: 10.29328/journal.ijceo.1001059; 9: 001-003
-
Metastatic Brain Melanoma: A Rare Case with Review of LiteratureNeha Singh,Gaurav Raj,Akshay Kumar,Deepak Kumar Singh,Shivansh Dixit,Kaustubh Gupta*. Metastatic Brain Melanoma: A Rare Case with Review of Literature. J Radiol Oncol. 2025: doi: ; 9: 050-053
-
Depression as a civilization-deformed adaptation and defence mechanismBohdan Wasilewski*,Olha Yourtsenyuk,Eugene Egan. Depression as a civilization-deformed adaptation and defence mechanism. Insights Depress Anxiety. 2020: doi: 10.29328/journal.ida.1001013; 4: 008-011
-
Drinking-water Quality Assessment in Selective Schools from the Mount LebanonWalaa Diab, Mona Farhat, Marwa Rammal, Chaden Moussa Haidar*, Ali Yaacoub, Alaa Hamzeh. Drinking-water Quality Assessment in Selective Schools from the Mount Lebanon. Ann Civil Environ Eng. 2024: doi: 10.29328/journal.acee.1001061; 8: 018-024
-
Rapid Microbial Growth in Reusable Drinking Water BottlesQishan Liu*,Hongjun Liu. Rapid Microbial Growth in Reusable Drinking Water Bottles. Ann Civil Environ Eng. 2017: doi: 10.29328/journal.acee.1001007; 1: 055-062
Most Viewed
-
Evaluation of Biostimulants Based on Recovered Protein Hydrolysates from Animal By-products as Plant Growth EnhancersH Pérez-Aguilar*, M Lacruz-Asaro, F Arán-Ais. Evaluation of Biostimulants Based on Recovered Protein Hydrolysates from Animal By-products as Plant Growth Enhancers. J Plant Sci Phytopathol. 2023 doi: 10.29328/journal.jpsp.1001104; 7: 042-047
-
Sinonasal Myxoma Extending into the Orbit in a 4-Year Old: A Case PresentationJulian A Purrinos*, Ramzi Younis. Sinonasal Myxoma Extending into the Orbit in a 4-Year Old: A Case Presentation. Arch Case Rep. 2024 doi: 10.29328/journal.acr.1001099; 8: 075-077
-
Feasibility study of magnetic sensing for detecting single-neuron action potentialsDenis Tonini,Kai Wu,Renata Saha,Jian-Ping Wang*. Feasibility study of magnetic sensing for detecting single-neuron action potentials. Ann Biomed Sci Eng. 2022 doi: 10.29328/journal.abse.1001018; 6: 019-029
-
Pediatric Dysgerminoma: Unveiling a Rare Ovarian TumorFaten Limaiem*, Khalil Saffar, Ahmed Halouani. Pediatric Dysgerminoma: Unveiling a Rare Ovarian Tumor. Arch Case Rep. 2024 doi: 10.29328/journal.acr.1001087; 8: 010-013
-
Physical activity can change the physiological and psychological circumstances during COVID-19 pandemic: A narrative reviewKhashayar Maroufi*. Physical activity can change the physiological and psychological circumstances during COVID-19 pandemic: A narrative review. J Sports Med Ther. 2021 doi: 10.29328/journal.jsmt.1001051; 6: 001-007

HSPI: We're glad you're here. Please click "create a new Query" if you are a new visitor to our website and need further information from us.
If you are already a member of our network and need to keep track of any developments regarding a question you have already submitted, click "take me to my Query."