Abstract
Research Article
Neuroprotective Effect of 7,8-dihydroxyflavone in a Mouse Model of HIV-Associated Neurocognitive Disorder (HAND)
Tapas K Makar, Joseph Bryant, Bosung Shim, Kaspar Keledjian, Harry Davis, Manik Ghosh, Ajay Koirala, Ishani Ghosh, Shreya Makar, Alonso Heredia, Malcolm Lane, J Marc Simard, Robert C Gallo, Volodymyr Gerzanich* and Istvan Merchenthaler*
Published: 18 September, 2024 | Volume 8 - Issue 2 | Pages: 090-105
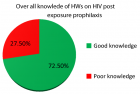
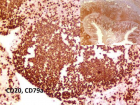
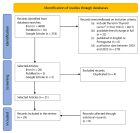
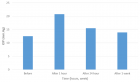
Treatment for HIV-associated neurocognitive disorders (HAND) remains elusive. 7,8-dihydroxyflavone (DHF), an analog of brain-derived neurotrophic factor (BDNF) and a high-affinity TrkB agonist, has been proposed as a viable therapeutic alternative to BDNF in crossing the Blood-Brain Barrier (BBB) and promoting growth, differentiation, maintenance, and survival of neurons. Here, we expand on our previous study investigating the therapeutic role of DHF on the cortical and hippocampal brain regions of the Tg26 mice, an animal model of HAND. We detected increased immunoreactivity for ion channels (SUR1, TRPM4) and the water channel aquaporin-4 (AQP4), suggesting an ionic and osmotic imbalance in the brains of Tg26 mice. Tg26 mice also exhibited loss of synaptic stability (SYN, SYP) and nicotinamide metabolism (NAMPT, SIRT1) that were associated with astrogliosis. Furthermore, Tg26 mice demonstrated increased iNOS and reduced HO-1/NRF2 expressions, implicating increased ER and oxidative stress. DHF treatment in Tg26 mice reversed these pathological changes. These data suggest crosstalk among TrkB, Akt, and related transcription factors (NF-κB, STAT3, and NRF2) as an underlying mechanism of Tg26-associated pathology in the brain. Finally, taken together with our prior study, these results further highlight a therapeutic role of DHF in promoting neuroprotection in HAND that may be applied in conjunction with current antiviral therapies.
Read Full Article HTML DOI: 10.29328/journal.jnnd.1001101 Cite this Article Read Full Article PDF
Keywords:
HAND; BDNF; TrkB; DHF; Transgenic; Transgenic mice-Tg26; Neurodegeneration; Neuroprotection; Antioxidant; Oxidative stress
References
- Tedaldi EM, Minniti NL, Fischer T. HIV-associated neurocognitive disorders: the relationship of HIV infection with physical and social comorbidities. Biomed Res Int. 2015;2015:5641913. Available from: https://doi.org/10.1155/2015/641913
- Sun W, Rassadkina Y, Gao C, Collens SI, Lian X, Solomon IH, et al. Persistence of intact HIV-1 proviruses in the brain during antiretroviral therapy. Elife. 2023;12. Available from: https://doi.org/10.7554/elife.89837
- Jadhav S, Nema V. HIV-Associated Neurotoxicity: The Interplay of Host and Viral Proteins. Mediators Inflamm. 2021;2021:1267041. Available from: https://doi.org/10.1155%2F2021%2F1267041
- Sanchez AB, Kaul M. Neuronal Stress and Injury Caused by HIV-1, cART and Drug Abuse: Converging Contributions to HAND. Brain Sci. 2017;7(3):33. Available from: https://doi.org/10.3390%2Fbrainsci7030025
- Evans DT, Silvestri G. Nonhuman primate models in AIDS research. Curr Opin HIV AIDS. 2013;8(4):255-61. Available from: https://doi.org/10.1097/coh.0b013e328361cee8
- Su H, Cheng Y, Sravanam S, Mathews S, Gorantla S, Poluektova LY, et al. Immune Activations and Viral Tissue Compartmentalization During Progressive HIV-1 Infection of Humanized Mice. Front Immunol. 2019;10:340. Available from: https://doi.org/10.3389%2Ffimmu.2019.00340
- Bar KJ, Coronado E, Hensley-McBain T, O'Connor MA, Osborn JM, Miller C, et al. Simian-Human Immunodeficiency Virus SHIV.CH505 Infection of Rhesus Macaques Results in Persistent Viral Replication and Induces Intestinal Immunopathology. J Virol. 2019;93(18). Available from: https://doi.org/10.1128%2FJVI.00372-19
- Horch HW, Katz LC. BDNF release from single cells elicits local dendritic growth in nearby neurons. Nat Neurosci. 2002;5(11):1177-84. Available from: https://doi.org/10.1038/nn927
- Nagahara AH, Merrill DA, Coppola G, Tsukada S, Schroeder BE, Shaked GM, et al. Neuroprotective effects of brain-derived neurotrophic factor in rodent and primate models of Alzheimer's disease. Nat Med. 2009;15(3):331-7. Available from: https://doi.org/10.1038/nm.1912
- Michael H, Mpofana T, Ramlall S, Oosthuizen F. The Role of Brain Derived Neurotrophic Factor in HIV-Associated Neurocognitive Disorder: From the Bench-Top to the Bedside. Neuropsychiatr Dis Treat. 2020;16:3557-67. Available from: https://doi.org/10.2147%2FNDT.S232836
- Abassi M, Morawski BM, Nakigozi G, Nakasujja N, Kong X, Meya DB, et al. Cerebrospinal fluid biomarkers and HIV-associated neurocognitive disorders in HIV-infected individuals in Rakai, Uganda. J Neurovirol. 2017;23(3):369-75. Available from: https://doi.org/10.1007%2Fs13365-016-0505-9
- Falasca K, Reale M, Ucciferri C, Di Nicola M, Di Martino G, D'Angelo C, et al. Cytokines, Hepatic Fibrosis, and Antiretroviral Therapy Role in Neurocognitive Disorders HIV Related. AIDS Res Hum Retroviruses. 2017;33(3):246-53. Available from: https://doi.org/10.1089/aid.2016.0138
- Dong XX, Wang Y, Qin ZH. Molecular mechanisms of excitotoxicity and their relevance to pathogenesis of neurodegenerative diseases. Acta Pharmacol Sin. 2009;30(4):379-87. Available from: https://www.nature.com/articles/aps200924
- Jang SW, Liu X, Yepes M, Shepherd KR, Miller GW, Liu Y, et al. A selective TrkB agonist with potent neurotrophic activities by 7,8-dihydroxyflavone. Proc Natl Acad Sci U S A. 2010;107(6):2687-92. Available from: https://doi.org/10.1073/pnas.0913572107
- Liu X, Qi Q, Xiao G, Li J, Luo HR, Ye K. O-methylated metabolite of 7,8-dihydroxyflavone activates TrkB receptor and displays antidepressant activity. Pharmacology. 2013;91(3-4):185-200. Available from: https://doi.org/10.1159%2F000346920
- Andero R, Daviu N, Escorihuela RM, Nadal R, Armario A. 7,8-dihydroxyflavone, a TrkB receptor agonist, blocks long-term spatial memory impairment caused by immobilization stress in rats. Hippocampus. 2012;22(3):399-408. Available from: https://doi.org/10.1002/hipo.20906
- Andero R, Heldt SA, Ye K, Liu X, Armario A, Ressler KJ. Effect of 7,8-dihydroxyflavone, a small-molecule TrkB agonist, on emotional learning. Am J Psychiatry. 2011;168(2):163-72. Available from: https://doi.org/10.1176/appi.ajp.2010.10030326
- Bryant J, Andhavarapu S, Bever C, Guda P, Katuri A, Gupta U, et al. 7,8-Dihydroxyflavone improves neuropathological changes in the brain of Tg26 mice, a model for HIV-associated neurocognitive disorder. Sci Rep. 2021;11(1):18519. Available from: https://doi.org/10.1038/s41598-021-97220-8
- Yang S, Zhu G. 7,8-Dihydroxyflavone and Neuropsychiatric Disorders: A Translational Perspective from the Mechanism to Drug Development. Curr Neuropharmacol. 2022;20(8):1479-97. Available from: https://doi.org/10.2174/1570159x19666210915122820
- Ton H, Xiong H. Astrocyte Dysfunctions and HIV-1 Neurotoxicity. J AIDS Clin Res. 2013;4(11):255. Available from: https://doi.org/10.4172%2F2155-6113.1000255
- Sofroniew MV, Vinters HV. Astrocytes: biology and pathology. Acta Neuropathol. 2010;119(1):7-35. Available from: https://doi.org/10.1007/s00401-009-0619-8
- Hubbard JA, Szu JI, Binder DK. The role of aquaporin-4 in synaptic plasticity, memory and disease. Brain Res Bull. 2018;136:118-29. Available from: https://doi.org/10.1016/j.brainresbull.2017.02.011
- Papadopoulos MC, Verkman AS. Aquaporin 4 and neuromyelitis optica. Lancet Neurol. 2012;11(6):535-44. Available from: https://doi.org/10.1016/s1474-4422(12)70133-3
- Verkman AS, Binder DK, Bloch O, Auguste K, Papadopoulos MC. Three distinct roles of aquaporin-4 in brain function revealed by knockout mice. Biochim Biophys Acta. 2006;1758(8):1085-93. Available from: https://doi.org/10.1016/j.bbamem.2006.02.018
- Simard JM, Woo SK, Schwartzbauer GT, Gerzanich V. Sulfonylurea receptor 1 in central nervous system injury: a focused review. J Cereb Blood Flow Metab. 2012;32(9):1699-717. Available from: https://doi.org/10.1038%2Fjcbfm.2012.91
- Cho CH, Lee YS, Kim E, Hwang EM, Park JY. Physiological functions of the TRPM4 channels via protein interactions. BMB Rep. 2015;48(1):1-5. Available from: https://doi.org/10.5483%2FBMBRep.2015.48.1.252
- Song SH, Augustine GJ. Synapsin Isoforms and Synaptic Vesicle Trafficking. Mol Cells. 2015;38(11):936-40. Available from: https://doi.org/10.14348%2Fmolcells.2015.0233
- Ellis R, Langford D, Masliah E. HIV and antiretroviral therapy in the brain: neuronal injury and repair. Nat Rev Neurosci. 2007;8(1):33-44. Available from: https://doi.org/10.1038/nrn2040
- James HJ, Sharer LR, Zhang Q, Wang HG, Epstein LG, Reed JC, et al. Expression of caspase-3 in brains from paediatric patients with HIV-1 encephalitis. Neuropathol Appl Neurobiol. 1999;25(5):380-6. Available from: https://doi.org/10.1046/j.1365-2990.1999.00195.x
- Zucker RS, Bennett M. Release of neurotransmitters. In: Zigmond MJ, Landis SC, Roberts JL, Squire LR, editors. Fundamental Neuroscience. San Diego: Academic Press; 1999;155-92.
- Sarnat HB, Flores-Sarnat L, Trevenen CL. Synaptophysin immunoreactivity in the human hippocampus and neocortex from 6 to 41 weeks of gestation. J Neuropathol Exp Neurol. 2010;69(3):234-45. Available from: https://doi.org/10.1097/nen.0b013e3181d0151f
- Revollo JR, Grimm AA, Imai S. The NAD biosynthesis pathway mediated by nicotinamide phosphoribosyltransferase regulates Sir2 activity in mammalian cells. J Biol Chem. 2004;279(49):50754-63. Available from: https://doi.org/10.1074/jbc.m408388200
- Lepeta K, Lourenco MV, Schweitzer BC, Martino Adami PV, Banerjee P, Catuara-Solarz S, et al. Synaptopathies: synaptic dysfunction in neurological disorders - A review from students to students. J Neurochem. 2016;138(6):785-805. Available from: https://doi.org/10.1111/jnc.13713
- Vreones M, Mustapic M, Moaddel R, Pucha KA, Lovett J, Seals DR, et al. Oral nicotinamide riboside raises NAD+ and lowers biomarkers of neurodegenerative pathology in plasma extracellular vesicles enriched for neuronal origin. Aging Cell. 2023;22(1). Available from: https://doi.org/10.1111/acel.13754
- Fujita Y, Yamashita T. Sirtuins in Neuroendocrine Regulation and Neurological Diseases. Front Neurosci. 2018;12:778. Available from: https://doi.org/10.3389%2Ffnins.2018.00778
- Figarola-Centurion I, Escoto-Delgadillo M, Gonzalez-Enriquez GV, Gutierrez-Sevilla JE, Vazquez-Valls E, Torres-Mendoza BM. Sirtuins Modulation: A Promising Strategy for HIV-Associated Neurocognitive Impairments. Int J Mol Sci. 2022;23(2):653. Available from: https://doi.org/10.3390/ijms23020643
- Chang Z, Wang Y, Zhou X, Long JE. STAT3 roles in viral infection: antiviral or proviral? Future Virol. 2018;13(8):557-74. Available from: https://doi.org/10.2217%2Ffvl-2018-0033
- Picon-Pages P, Garcia-Buendia J, Munoz FJ. Functions and dysfunctions of nitric oxide in brain. Biochim Biophys Acta Mol Basis Dis. 2019;1865(8):1949-67. Available from: https://doi.org/10.1016/j.bbadis.2018.11.007
- Vincent VA, De Groot CJ, Lucassen PJ, Portegies P, Troost D, Tilders FJ, et al. Nitric oxide synthase expression and apoptotic cell death in brains of AIDS and AIDS dementia patients. AIDS. 1999;13(3):317-26. Available from: https://doi.org/10.1097/00002030-199902250-00003
- Nitti M, Piras S, Brondolo L, Marinari UM, Pronzato MA, Furfaro AL. Heme Oxygenase 1 in the Nervous System: Does It Favor Neuronal Cell Survival or Induce Neurodegeneration? Int J Mol Sci. 2018;19(8):2354. Available from: https://doi.org/10.3390%2Fijms19082260
- Singh S, Nagalakshmi D, Sharma KK, Ravichandiran V. Natural antioxidants for neuroinflammatory disorders and possible involvement of Nrf2 pathway: A review. Heliyon. 2021;7(2). Available from: https://doi.org/10.1016%2Fj.heliyon.2021.e06216
- Tang H, Lu D, Pan R, Qin X, Xiong H, Dong J. Curcumin improves spatial memory impairment induced by human immunodeficiency virus type 1 glycoprotein 120 V3 loop peptide in rats. Life Sci. 2009;85(1-2):1-10. Available from: https://doi.org/10.1016/j.lfs.2009.03.013
- Souza-Junior FJC, Lisboa SF. Toll-like receptor 4 in the interface between neuroimmune response and behavioral alterations caused by stress. Exploration of Neuroprotective Therapy. Exploration of Neuroprotective Therapy. 2022;(2):182-209. Available from: https://doi.org/10.37349/ent.2022.00028
- Nickoloff-Bybel EA, Festa L, Meucci O, Gaskill PJ. Co-receptor signaling in the pathogenesis of neuroHIV. Retrovirology. 2021;18(1):24. Available from: https://retrovirology.biomedcentral.com/articles/10.1186/s12977-021-00569-x
- Wahl A, Al-Harthi L. HIV infection of non-classical cells in the brain. Retrovirology. 2023;20(1):1. Available from: https://retrovirology.biomedcentral.com/articles/10.1186/s12977-023-00616-9
- Li G, Makar T, Gerzanich V, Kalakonda S, Ivanova S, Pereira EFR, et al. HIV-1 Vpr-Induced Proinflammatory Response and Apoptosis Are Mediated through the SUR1-TRPM4 Channel in Astrocytes. mBio. 2020;11(6). Available from: https://doi.org/10.1128/mbio.02939-20
- Keledjian K, Makar T, Zhang C, Zhang J, Shim B, Davis H, et al. Correlation of HIV-Induced Neuroinflammation and Synaptopathy with Impairment of Learning and Memory in Mice with HAND. J Clin Med. 2023;12(16). Available from: https://doi.org/10.3390%2Fjcm12165169
- Barbe MF, Loomis R, Lepkowsky AM, Forman S, Zhao H, Gordon J. A longitudinal characterization of sex-specific somatosensory and spatial memory deficits in HIV Tg26 heterozygous mice. PLoS One. 2020;15(12). Available from: https://doi.org/10.1371/journal.pone.0244725
- Stokum JA, Kurland DB, Gerzanich V, Simard JM. Mechanisms of astrocyte-mediated cerebral edema. Neurochem Res. 2015;40(2):317-28. Available from: https://doi.org/10.1007/s11064-014-1374-3
- Stokum JA, Kwon MS, Woo SK, Tsymbalyuk O, Vennekens R, Gerzanich V, et al. SUR1-TRPM4 and AQP4 form a heteromultimeric complex that amplifies ion/water osmotic coupling and drives astrocyte swelling. Glia. 2018;66(1):108-25. Available from: https://doi.org/10.1002%2Fglia.23231
- Verkhratsky A, Butt A, Li B, Illes P, Zorec R, Semyanov A, et al. Astrocytes in human central nervous system diseases: a frontier for new therapies. Signal Transduct Target Ther. 2023;8(1):396. Available from: https://www.nature.com/articles/s41392-023-01628-9
- Mahmoud S, Gharagozloo M, Simard C, Gris D. Astrocytes Maintain Glutamate Homeostasis in the CNS by Controlling the Balance between Glutamate Uptake and Release. Cells. 2019;8(2):234. Available from: https://doi.org/10.3390%2Fcells8020184
- Blum R, Kafitz KW, Konnerth A. Neurotrophin-evoked depolarization requires the sodium channel Na(V)1.9. Nature. 2002;419(6908):687-93. Available from: https://doi.org/10.1038/nature01085
- Tucker K, Fadool DA. Neurotrophin modulation of voltage-gated potassium channels in rat through TrkB receptors is time and sensory experience dependent. J Physiol. 2002;542(Pt 2):413-29. Available from: https://doi.org/10.1113/jphysiol.2002.017376
- Colley BS, Biju KC, Visegrady A, Campbell S, Fadool DA. Neurotrophin B receptor kinase increases Kv subfamily member 1.3 (Kv1.3) ion channel half-life and surface expression. Neuroscience. 2007;144(2):531-46. Available from: https://doi.org/10.1016/j.neuroscience.2006.09.055
- Colley BS, Cavallin MA, Biju K, Marks DR, Fadool DA. Brain-derived neurotrophic factor modulation of Kv1.3 channel is disregulated by adaptor proteins Grb10 and nShc. BMC Neurosci. 2009;10:108. Available from: https://doi.org/10.1186%2F1471-2202-10-8
- Liu QH, Williams DA, McManus C, Baribaud F, Doms RW, Schols D, et al. HIV-1 gp120 and chemokines activate ion channels in primary macrophages through CCR5 and CXCR4 stimulation. Proc Natl Acad Sci U S A. 2000;97(9):4832-7. Available from: https://doi.org/10.1073%2Fpnas.090521697
- Lin G, Baribaud F, Romano J, Doms RW, Hoxie JA. Identification of gp120 binding sites on CXCR4 by using CD4-independent human immunodeficiency virus type 2 Env proteins. J Virol. 2003;77(2):931-42. Available from: https://doi.org/10.1128%2FJVI.77.2.931-942.2003
- Cosme D, Soares-da-Silva P, Magro F. Effect of Toll-like receptor-2, -4, -5, -7, and NOD2 stimulation on potassium channel conductance in intestinal epithelial cells. Am J Physiol Gastrointest Liver Physiol. 2022;323(5). Available https://doi.org/10.1152/ajpgi.00139.2022
- Di Liberto G, Egervari K, Kreutzfeldt M, Schurch CM, Hewer E, Wagner I, et al. Neurodegenerative phagocytes mediate synaptic stripping in Neuro-HIV. Brain. 2022;145(8):2730-41. Available from: https://doi.org/10.1093/brain/awac102
- Miranda M, Morici JF, Zanoni MB, Bekinschtein P. Brain-Derived Neurotrophic Factor: A Key Molecule for Memory in the Healthy and the Pathological Brain. Front Cell Neurosci. 2019;13:363. Available from: https://doi.org/10.3389%2Ffncel.2019.00363
- Bachis A, Adams AV, Lim ST, Mocchetti I. Neurotrophic Factors and NeuroAIDS: A Lesson from Brain-Derived Neurotrophic Factor. New York, NY: Springer. 2014.
- Vitaliano GD, Kim JK, Kaufman MJ, Adam CW, Zeballos G, Shanmugavadivu A, et al. Clathrin-nanoparticles deliver BDNF to hippocampus and enhance neurogenesis, synaptogenesis and cognition in HIV/neuroAIDS mouse model. Commun Biol. 2022;5(1):236. Available from: https://doi.org/10.1038/s42003-022-03177-3
- Rosa JM, Farre-Alins V, Ortega MC, Navarrete M, Lopez-Rodriguez AB, Palomino-Antolin A, et al. TLR4 pathway impairs synaptic number and cerebrovascular functions through astrocyte activation following traumatic brain injury. Br J Pharmacol. 2021;178(17):3395-413. Available from: https://doi.org/10.1111/bph.15488
- Friedman-Levi Y, Liraz-Zaltsman S, Shemesh C, Rosenblatt K, Kesner EL, Gincberg G, et al. Pharmacological blockers of CCR5 and CXCR4 improve recovery after traumatic brain injury. Exp Neurol. 2021;338:113604. Available from: https://doi.org/10.1016/j.expneurol.2021.113604
- Necula D, Riviere-Cazaux C, Shen Y, Zhou M. Insight into the roles of CCR5 in learning and memory in normal and disordered states. Brain Behav Immun. 2021;92:1-9. Available from: https://doi.org/10.1016/j.bbi.2020.11.037
- Zhang Z, Liu X, Schroeder JP, Chan CB, Song M, Yu SP, et al. 7,8-dihydroxyflavone prevents synaptic loss and memory deficits in a mouse model of Alzheimer's disease. Neuropsychopharmacology. 2014;39(3):638-50. Available from: https://doi.org/10.1038/npp.2013.243
- Zeng Y, Liu Y, Wu M, Liu J, Hu Q. Activation of TrkB by 7,8-dihydroxyflavone prevents fear memory defects and facilitates amygdalar synaptic plasticity in aging. J Alzheimers Dis. 2012;31(4):765-78. Available from: https://doi.org/10.3233/jad-2012-120886
- Canto C, Menzies KJ, Auwerx J. NAD(+) Metabolism and the Control of Energy Homeostasis: A Balancing Act between Mitochondria and the Nucleus. Cell Metab. 2015;22(1):31-53. Available from: https://doi.org/10.1016%2Fj.cmet.2015.05.023
- Elhassan YS, Kluckova K, Fletcher RS, Schmidt MS, Garten A, Doig CL, et al. Nicotinamide Riboside Augments the Aged Human Skeletal Muscle NAD(+) Metabolome and Induces Transcriptomic and Anti-inflammatory Signatures. Cell Rep. 2019;28(7):1717-28.e6. Available from: https://doi.org/10.1016/j.celrep.2019.07.043
- Rajman L, Chwalek K, Sinclair DA. Therapeutic Potential of NAD-Boosting Molecules: The In Vivo Evidence. Cell Metab. 2018;27(3):529-47. Available from: https://doi.org/10.1016%2Fj.cmet.2018.02.011
- Camacho-Pereira J, Tarrago MG, Chini CCS, Nin V, Escande C, Warner GM, et al. CD38 Dictates Age-Related NAD Decline and Mitochondrial Dysfunction through an SIRT3-Dependent Mechanism. Cell Metab. 2016;23(6):1127-39. Available from: https://doi.org/10.1016/j.cmet.2016.05.006
- Brakedal B, Dolle C, Riemer F, Ma Y, Nido GS, Skeie GO, et al. The NADPARK study: A randomized phase I trial of nicotinamide riboside supplementation in Parkinson's disease. Cell Metab. 2022;34(3):396-407.e6. Available from: https://doi.org/10.1016/j.cmet.2022.02.001
- Li C, Wu LE. Risks and rewards of targeting NAD(+) homeostasis in the brain. Mech Ageing Dev. 2021;198:111545. Available from: https://doi.org/10.1016/j.mad.2021.111545
- Groth B, Venkatakrishnan P, Lin SJ. NAD(+) Metabolism, Metabolic Stress, and Infection. Front Mol Biosci. 2021;8:686412. Available from: https://doi.org/10.3389/fmolb.2021.686412
- Chen XY, Zhang HS, Wu TC, Sang WW, Ruan Z. Down-regulation of NAMPT expression by miR-182 is involved in Tat-induced HIV-1 long terminal repeat (LTR) transactivation. Int J Biochem Cell Biol. 2013;45(2):292-8. Available from: https://doi.org/10.1016/j.biocel.2012.11.002
- Yeung F, Hoberg JE, Ramsey CS, Keller MD, Jones DR, Frye RA, et al. Modulation of NF-kappaB-dependent transcription and cell survival by the SIRT1 deacetylase. EMBO J. 2004;23(12):2369-80. Available from: https://doi.org/10.1038/sj.emboj.7600244
- Castro V, Bertrand L, Luethen M, Dabrowski S, Lombardi J, Morgan L, et al. Occludin controls HIV transcription in brain pericytes via regulation of SIRT-1 activation. FASEB J. 2016;30(3):1234-46. Available from: https://doi.org/10.1096/fj.15-277673
- Sharma P, Silva C, Pfreundschuh S, Ye H, Sampath H. Metabolic protection by the dietary flavonoid 7,8-dihydroxyflavone requires an intact gut microbiome. Front Nutr. 2022;9:987956. Available from: https://doi.org/10.3389%2Ffnut.2022.987956
- Gambini J, Ingles M, Olaso G, Lopez-Grueso R, Bonet-Costa V, Gimeno-Mallench L, et al. Properties of Resveratrol: In Vitro and In Vivo Studies about Metabolism, Bioavailability, and Biological Effects in Animal Models and Humans. Oxid Med Cell Longev. 2015;2015:837042. Available from: https://doi.org/10.1155/2015/837042
- Fan Y, Timani KA, He JJ. STAT3 and its phosphorylation are involved in HIV-1 Tat-induced transactivation of glial fibrillary acidic protein. Curr HIV Res. 2015;13(1):55-63. Available from: https://doi.org/10.2174%2F1570162x13666150121115804
- Yan J, Tang X, Zhou ZQ, Zhang J, Zhao Y, Li S, et al. Sirtuins functions in central nervous system cells under neurological disorders. Front Physiol. 2022;13:886087. Available from: https://doi.org/10.3389%2Ffphys.2022.886087
- Song Y, Wu Z, Zhao P. The protective effects of activating Sirt1/NF-kappaB pathway for neurological disorders. Rev Neurosci. 2022;33(4):427-38. Available from: https://doi.org/10.1515/revneuro-2021-0118
- Wang J, Zheng B, Yang S, Zhou D, Wang J. Olmesartan Prevents Oligomerized Amyloid beta (Abeta)-Induced Cellular Senescence in Neuronal Cells. ACS Chem Neurosci. 2021;12(7):1162-9. Available from: https://doi.org/10.1021/acschemneuro.0c00775
- Corpas R, Revilla S, Ursulet S, Castro-Freire M, Kaliman P, Petegnief V, et al. SIRT1 Overexpression in Mouse Hippocampus Induces Cognitive Enhancement Through Proteostatic and Neurotrophic Mechanisms. Mol Neurobiol. 2017;54(7):5604-19. Available from: https://doi.org/10.1007/s12035-016-0087-9
- Zhou Y, Wang S, Li Y, Yu S, Zhao Y. SIRT1/PGC-1alpha Signaling Promotes Mitochondrial Functional Recovery and Reduces Apoptosis after Intracerebral Hemorrhage in Rats. Front Mol Neurosci. 2017;10:443. Available from: https://doi.org/10.3389/fnmol.2017.00443
- Michan S, Li Y, Chou MM, Parrella E, Ge H, Long JM, et al. SIRT1 is essential for normal cognitive function and synaptic plasticity. J Neurosci. 2010;30(29):9695-707. Available from: https://doi.org/10.1523%2FJNEUROSCI.0027-10.2010
- Louboutin JP, Strayer D. Role of Oxidative Stress in HIV-1-Associated Neurocognitive Disorder and Protection by Gene Delivery of Antioxidant Enzymes. Antioxidants (Basel). 2014;3(4):770-97. Available from: https://doi.org/10.3390%2Fantiox3040770
- Shah S, Maric D, Denaro F, Ibrahim W, Mason R, Kumar A, et al. Nitrosative Stress Is Associated with Dopaminergic Dysfunction in the HIV-1 Transgenic Rat. Am J Pathol. 2019;189(7):1375-85. Available from: https://doi.org/10.1016%2Fj.ajpath.2019.03.004
- Goodkin K, Miller EN, Cox C, Reynolds S, Becker JT, Martin E, et al. Effect of ageing on neurocognitive function by stage of HIV infection: evidence from the Multicenter AIDS Cohort Study. Lancet HIV. 2017;4(9). Available from: https://doi.org/10.1016/s2352-3018(17)30098-x
- Goodkin K, Wilkie FL, Concha M, Hinkin CH, Symes S, Baldewicz TT, et al. Aging and neuro-AIDS conditions and the changing spectrum of HIV-1-associated morbidity and mortality. J Clin Epidemiol. 2001;54 Suppl 1. Available https://doi.org/10.1016/s0895-4356(01)00445-0
- Fields J, Dumaop W, Langford TD, Rockenstein E, Masliah E. Role of neurotrophic factor alterations in the neurodegenerative process in HIV associated neurocognitive disorders. J Neuroimmune Pharmacol. 2014;9(2):102-16. Available from: https://doi.org/10.1007/s11481-013-9520-2
- Dinkova-Kostova AT, Abramov AY. The emerging role of Nrf2 in mitochondrial function. Free Radic Biol Med. 2015;88(Pt B):179-88. Available from: https://doi.org/10.1016%2Fj.freeradbiomed.2015.04.036
- Cassina A, Radi R. Differential inhibitory action of nitric oxide and peroxynitrite on mitochondrial electron transport. Arch Biochem Biophys. 1996;328(2):309-16. Available from: https://doi.org/10.1006/abbi.1996.0178
- Torre D, Pugliese A, Speranza F. Role of nitric oxide in HIV-1 infection: friend or foe? Lancet Infect Dis. 2002;2(5):273-80. Available from: https://doi.org/10.1016/s1473-3099(02)00262-1
- Hori K, Burd PR, Furuke K, Kutza J, Weih KA, Clouse KA. Human immunodeficiency virus-1-infected macrophages induce inducible nitric oxide synthase and nitric oxide (NO) production in astrocytes: astrocytic NO as a possible mediator of neural damage in acquired immunodeficiency syndrome. Blood. 1999;93(6):1843-50. Available from: https://pubmed.ncbi.nlm.nih.gov/10068656/
- Ryter SW, Choi AM. Targeting heme oxygenase-1 and carbon monoxide for therapeutic modulation of inflammation. Transl Res. 2016;167(1):7-34. Available from: https://doi.org/10.1016/j.trsl.2015.06.011
- Srisook K, Cha YN. Super-induction of HO-1 in macrophages stimulated with lipopolysaccharide by prior depletion of glutathione decreases iNOS expression and NO production. Nitric Oxide. 2005;12(2):70-9. Available from: https://doi.org/10.1016/j.niox.2004.12.002
- Srisook K, Kim C, Cha YN. Cytotoxic and cytoprotective actions of O2- and NO (ONOO-) are determined both by cellular GSH level and HO activity in macrophages. Methods Enzymol. 2005;396:414-24. Available from: https://doi.org/10.1016/s0076-6879(05)96035-7
- Ambegaokar SS, Kolson DL. Heme oxygenase-1 dysregulation in the brain: implications for HIV-associated neurocognitive disorders. Curr HIV Res. 2014;12(3):174-88. Available from: https://doi.org/10.2174%2F1570162X12666140526122709
- Huang Y, Wu L, Xu C, Yang B, Wang R. Increased HO-1 expression and decreased iNOS expression in the hippocampus from adult spontaneously hypertensive rats. Cell Biochem Biophys. 2006;46(1):35-42. Available from: https://link.springer.com/article/10.1385/CBB:46:1:35
- Han D, Lu X, Yin W, Fu H, Zhang X, Cheng L, et al. Activation of NRF2 blocks HIV replication and apoptosis in macrophages. Heliyon. 2023;9(1). Available from: https://doi.org/10.1016%2Fj.heliyon.2022.e12575
- Linker RA, Lee DH, Ryan S, van Dam AM, Conrad R, Bista P, et al. Fumaric acid esters exert neuroprotective effects in neuroinflammation via activation of the Nrf2 antioxidant pathway. Brain. 2011;134(Pt 3):678-92. Available from: https://doi.org/10.1093/brain/awq386
- Gill AJ, Kovacsics CE, Cross SA, Vance PJ, Kolson LL, Jordan-Sciutto KL, et al. Heme oxygenase-1 deficiency accompanies neuropathogenesis of HIV-associated neurocognitive disorders. J Clin Invest. 2014;124(10):4459-72. Available from: https://doi.org/10.1172/jci72279
- Roach JP, Moore EE, Partrick DA, Damle SS, Silliman CC, McIntyre RC Jr, et al. Heme oxygenase-1 induction in macrophages by a hemoglobin-based oxygen carrier reduces endotoxin-stimulated cytokine secretion. Shock. 2009;31(3):251-7. Available from: https://doi.org/10.1097/shk.0b013e3181834115
- Pittock ST, Norby SM, Grande JP, Croatt AJ, Bren GD, Badley AD, et al. MCP-1 is up-regulated in unstressed and stressed HO-1 knockout mice: Pathophysiologic correlates. Kidney Int. 2005;68(2):611-22. Available from: https://doi.org/10.1111/j.1523-1755.2005.00439.x
- Pandey SN, Kwatra M, Dwivedi DK, Choubey P, Lahkar M, Jangra A. 7,8-Dihydroxyflavone alleviated the high-fat diet and alcohol-induced memory impairment: behavioral, biochemical and molecular evidence. Psychopharmacology (Berl). 2020;237(6):1827-40. Available from: https://doi.org/10.1007/s00213-020-05502-2
- Wang S, Ding X, Li Z, Rao F, Xu H, Lu J, et al. Comprehensive analyses identify potential biomarkers for encephalitis in HIV infection. Sci Rep. 2023;13(1):18418. Available from: https://doi.org/10.1038/s41598-023-45922-6
- Chen C, Ahn EH, Kang SS, Liu X, Alam A, Ye K. Gut dysbiosis contributes to amyloid pathology, associated with C/EBPbeta/AEP signaling activation in Alzheimer's disease mouse model. Sci Adv. 2020;6(31). Available from: https://doi.org/10.1126/sciadv.aba0466
- He J, Xiang Z, Zhu X, Ai Z, Shen J, Huang T, et al. Neuroprotective Effects of 7,8-dihydroxyflavone on Midbrain Dopaminergic Neurons in MPP(+)-treated Monkeys. Sci Rep. 2016;6:34339. Available from: https://www.nature.com/articles/srep34339
- Kamarudin MNA, Sarker MMR, Zhou JR, Parhar I. Metformin in colorectal cancer: molecular mechanism, preclinical and clinical aspects. J Exp Clin Cancer Res. 2019;38(1):491. Available from: https://doi.org/10.1186/s13046-019-1495-2
- Dickie P, Felser J, Eckhaus M, Bryant J, Silver J, Marinos N, et al. HIV-associated nephropathy in transgenic mice expressing HIV-1 genes. Virology. 1991;185(1):109-19. Available from: https://doi.org/10.1016/0042-6822(91)90759-5
- Curreli S, Krishnan S, Reitz M, Lunardi-Iskandar Y, Lafferty MK, Garzino-Demo A, et al. B cell lymphoma in HIV transgenic mice. Retrovirology. 2013;10:92. Available from: https://doi.org/10.1186/1742-4690-10-92
- Jaehne EJ, Chong EMS, Sbisa A, Gillespie B, Hill R, Gogos A, et al. TrkB agonist 7,8-dihydroxyflavone reverses an induced prepulse inhibition deficit selectively in maternal immune activation offspring: implications for schizophrenia. Behav Pharmacol. 2021;32(5):404-12. Available from: https://doi.org/10.1097/fbp.0000000000000632
- Wang N, Liu X, Li XT, Li XX, Ma W, Xu YM, et al. 7,8-Dihydroxyflavone Alleviates Anxiety-Like Behavior Induced by Chronic Alcohol Exposure in Mice Involving Tropomyosin-Related Kinase B in the Amygdala. Mol Neurobiol. 2021;58(1):92-105. Available from: https://doi.org/10.1007/s12035-020-02111-0
- Wang Z, Wang SP, Shao Q, Li PF, Sun Y, Luo LZ, et al. Brain-derived neurotrophic factor mimetic, 7,8-dihydroxyflavone, protects against myocardial ischemia by rebalancing optic atrophy 1 processing. Free Radic Biol Med. 2019;145:187-97. Available from: https://doi.org/10.1016/j.freeradbiomed.2019.09.033
- Garcia-Diaz Barriga G, Giralt A, Anglada-Huguet M, Gaja-Capdevila N, Orlandi JG, Soriano J, et al. 7,8-dihydroxyflavone ameliorates cognitive and motor deficits in a Huntington's disease mouse model through specific activation of the PLCgamma1 pathway. Hum Mol Genet. 2017;26(16):3144-60. Available from: https://doi.org/10.1093/hmg/ddx198
- Stagni F, Uguagliati B, Emili M, Giacomini A, Bartesaghi R, Guidi S. The flavonoid 7,8-DHF fosters prenatal brain proliferation potency in a mouse model of Down syndrome. Sci Rep. 2021;11(1):6300. Available from: https://doi.org/10.1038/s41598-021-85284-5
Figures:
Similar Articles
-
Vigour of CRISPR/Cas9 Gene Editing in Alzheimer’s DiseaseJes Paul*. Vigour of CRISPR/Cas9 Gene Editing in Alzheimer’s Disease. . 2018 doi: 10.29328/journal.jnnd.1001014; 2: 047-051
-
Carbonic Anhydrase I modifies SOD1-induced motor neuron toxicity in Drosophila via ER stress pathwayJian Liu*,Deyi Lu,Xiao Peng,Xuejiao Jia,Guiyi Li,Na Tan,Zhen Wei,Xinzhu Fei,Xiaochen Liu,Tatsuhiko Kadowaki,Jian Liu. Carbonic Anhydrase I modifies SOD1-induced motor neuron toxicity in Drosophila via ER stress pathway. . 2019 doi: 10.29328/journal.jnnd.1001024; 3: 135-144
-
Protection from the Pathogenesis of Neurodegenerative Disorders, including Alzheimer’s Disease, Amyotrophic Lateral Sclerosis, Huntington’s Disease, and Parkinson’s Diseases, through the Mitigation of Reactive Oxygen SpeciesSamskruthi Madireddy*,Sahithi Madireddy. Protection from the Pathogenesis of Neurodegenerative Disorders, including Alzheimer’s Disease, Amyotrophic Lateral Sclerosis, Huntington’s Disease, and Parkinson’s Diseases, through the Mitigation of Reactive Oxygen Species. . 2019 doi: 10.29328/journal.jnnd.1001026; 3: 148-161
-
Do genes matter in sleep?-A comprehensive updateRajib Dutta*. Do genes matter in sleep?-A comprehensive update. . 2020 doi: 10.29328/journal.jnnd.1001029; 4: 014-023
-
Impact of mandibular advancement device in quantitative electroencephalogram and sleep quality in mild to severe obstructive sleep apneaCuspineda-Bravo ER*,García- Menéndez M,Castro-Batista F,Barquín-García SM,Cadelo-Casado D,Rodríguez AJ,Sharkey KM. Impact of mandibular advancement device in quantitative electroencephalogram and sleep quality in mild to severe obstructive sleep apnea. . 2020 doi: 10.29328/journal.jnnd.1001041; 4: 088-098
-
Role of neuron specific enolase as a biomarker in Parkinson’s diseaseRajib Dutta*. Role of neuron specific enolase as a biomarker in Parkinson’s disease. . 2021 doi: 10.29328/journal.jnnd.1001052; 5: 061-068
-
Differential roles of trithorax protein MLL-1 in regulating neuronal Ion channelsSonya Dave,An Zhou*. Differential roles of trithorax protein MLL-1 in regulating neuronal Ion channels. . 2021 doi: 10.29328/journal.jnnd.1001057; 5: 089-093
-
Neurotoxicity related exposure to ambient nanoparticlesMojtaba Ehsanifar*,Zeinab Montazeri,Mehravar Rafati. Neurotoxicity related exposure to ambient nanoparticles. . 2022 doi: 10.29328/journal.jnnd.1001060; 6: 005-010
-
Nutritional interventions for the prevention and treatment of neurological disorders such as anxiety, bipolar disorder, depression, epilepsy, multiple sclerosis, and schizophreniaSahithi Madireddy*,Samskruthi Madireddy. Nutritional interventions for the prevention and treatment of neurological disorders such as anxiety, bipolar disorder, depression, epilepsy, multiple sclerosis, and schizophrenia. . 2022 doi: 10.29328/journal.jnnd.1001070; 6: 052-071
-
Case study (A and B): a patient with Parkinson’s diseaseMuhammad Zulkifl Hasan*,Muhammad Zunnurain Hussain,Khadeeja Anjum,Arha Anwar. Case study (A and B): a patient with Parkinson’s disease. . 2023 doi: 10.29328/journal.jnnd.1001073; 7: 005-010
Recently Viewed
-
FITT-CORRECT: Updated dynamic and evidence-based principle of exercise prescriptionShambhu P Adhikari*,Jarugool Tretriluxana,Rubee Dev,Emily Eglitis,Nistha Shrestha,Cheryl Kerfeld6. FITT-CORRECT: Updated dynamic and evidence-based principle of exercise prescription. J Nov Physiother Rehabil. 2021: doi: 10.29328/journal.jnpr.1001039; 5: 005-009
-
Cystoid Macular Oedema Secondary to Bimatoprost in a Patient with Primary Open Angle GlaucomaKonstantinos Kyratzoglou*,Katie Morton. Cystoid Macular Oedema Secondary to Bimatoprost in a Patient with Primary Open Angle Glaucoma. Int J Clin Exp Ophthalmol. 2025: doi: 10.29328/journal.ijceo.1001059; 9: 001-003
-
Sex after Neurosurgery–Limitations, Recommendations, and the Impact on Patient’s Well-beingMor Levi Rivka*, Csaba L Dégi. Sex after Neurosurgery–Limitations, Recommendations, and the Impact on Patient’s Well-being. J Neurosci Neurol Disord. 2024: doi: 10.29328/journal.jnnd.1001099; 8: 064-068
-
Physiotherapy Undergraduate Students’ Perception About Clinical Education; A Qualitative StudyPravakar Timalsina*,Bimika Khadgi. Physiotherapy Undergraduate Students’ Perception About Clinical Education; A Qualitative Study. J Nov Physiother Rehabil. 2024: doi: 10.29328/journal.jnpr.1001063; 8: 043-052
-
Clinical Significance of Anterograde Angiography for Preoperative Evaluation in Patients with Varicose VeinsYi Liu,Dong Liu#,Junchen Li#,Tianqing Yao,Yincheng Ran,Ke Tian,Haonan Zhou,Lei Zhou,Zhumin Cao*,Kai Deng*. Clinical Significance of Anterograde Angiography for Preoperative Evaluation in Patients with Varicose Veins. J Radiol Oncol. 2025: doi: 10.29328/journal.jro.1001073; 9: 001-006
Most Viewed
-
Evaluation of Biostimulants Based on Recovered Protein Hydrolysates from Animal By-products as Plant Growth EnhancersH Pérez-Aguilar*, M Lacruz-Asaro, F Arán-Ais. Evaluation of Biostimulants Based on Recovered Protein Hydrolysates from Animal By-products as Plant Growth Enhancers. J Plant Sci Phytopathol. 2023 doi: 10.29328/journal.jpsp.1001104; 7: 042-047
-
Sinonasal Myxoma Extending into the Orbit in a 4-Year Old: A Case PresentationJulian A Purrinos*, Ramzi Younis. Sinonasal Myxoma Extending into the Orbit in a 4-Year Old: A Case Presentation. Arch Case Rep. 2024 doi: 10.29328/journal.acr.1001099; 8: 075-077
-
Feasibility study of magnetic sensing for detecting single-neuron action potentialsDenis Tonini,Kai Wu,Renata Saha,Jian-Ping Wang*. Feasibility study of magnetic sensing for detecting single-neuron action potentials. Ann Biomed Sci Eng. 2022 doi: 10.29328/journal.abse.1001018; 6: 019-029
-
Pediatric Dysgerminoma: Unveiling a Rare Ovarian TumorFaten Limaiem*, Khalil Saffar, Ahmed Halouani. Pediatric Dysgerminoma: Unveiling a Rare Ovarian Tumor. Arch Case Rep. 2024 doi: 10.29328/journal.acr.1001087; 8: 010-013
-
Physical activity can change the physiological and psychological circumstances during COVID-19 pandemic: A narrative reviewKhashayar Maroufi*. Physical activity can change the physiological and psychological circumstances during COVID-19 pandemic: A narrative review. J Sports Med Ther. 2021 doi: 10.29328/journal.jsmt.1001051; 6: 001-007

HSPI: We're glad you're here. Please click "create a new Query" if you are a new visitor to our website and need further information from us.
If you are already a member of our network and need to keep track of any developments regarding a question you have already submitted, click "take me to my Query."